Background: Prolonged length of stay (LOS) is associated with worse quality outcomes, poor patient satisfaction, and negative financial performance for hospitals. Geographic cohorting of provider teams and their patients could improve LOS, readmissions, and other quality metrics. Many prior studies of geographic cohorting have shown no beneficial effect on these metrics. In 2021, we implemented a bundled intervention of geographic cohorting of patients and providers with structured multidisciplinary rounds (MDR) and additional case management (CM) support. We report the estimated effect on LOS, readmissions, estimated discharge date (EDD) accuracy, and discharge timing.
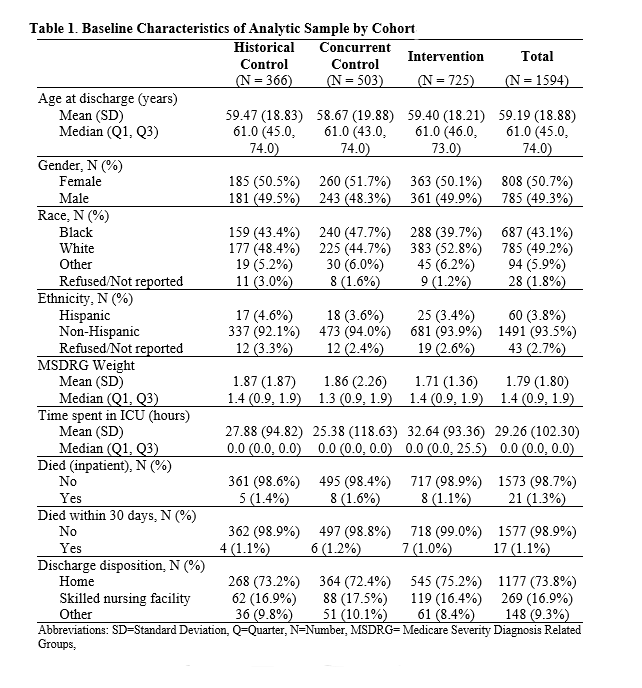
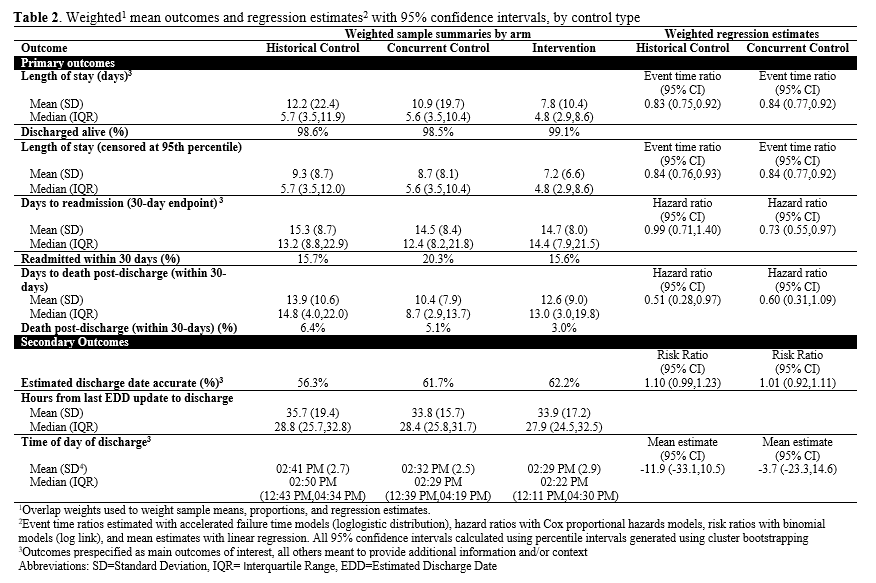
Methods: Quality Improvement Study at one academic hospital April to September 2021 evaluating geographic localization of adult hospital medicine inpatients and providers on a single unit, with twice daily MDRs and additional CM support. Comparison groups were same unit historical control (October 2020-March 2021) and concurrent control (2 other similar medicine units) (Table 1). Patients were cared for by non-teaching hospitalist teams comprised of MD and APP providers. Primary outcomes were hospital LOS and 30-day health system readmission. Secondary outcomes were accuracy of estimated discharge date (EDD) and discharge time of day.Propensity score weighting was used to balance sociodemographic and clinical characteristics between arms. LOS was analyzed using accelerated failure time models. Rates of 30-day hospital readmission were analyzed using Cox proportional hazard models. Accuracy of EDD was analyzed using log-binomial risk models. Time of day was analyzed using linear regression.
Results: Our study included 1594 discharge encounters, 725 discharges from the intervention unit during the study time period, 503 from the concurrent control, and 366 from the historical control. Median LOS was shorter for patients in the intervention group (4.8 days) as compared to the concurrent control (5.6 days), or the historic control (5.7 days). By event time analysis, LOS was 16% shorter in the intervention groups than both controls (event time ratio (ETR)=0.83, 95% CI: 0.75 – 0.92 for historical control; ETR=0.84, 95% CI: 0.77 – 0.92 for concurrent control) (Table 2). 30-day readmission rates were similar between the intervention and historical control (HR=0.99, 95% CI: 0.71 – 1.40), and lower than the concurrent control (16.5% vs 20.3%, HR=0.73, 95% CI: 0.55 – 0.97). The EDD was not significantly different between groups. There was little evidence of a difference in time of day of discharge. Patients with an ICU stay had a significantly increased odds of being in the intervention arm vs the control groups.
Conclusions: On a single general medicine unit with non-resident providers, a bundled intervention of geographic cohorting, in addition to structured multidisciplinary rounds and additional CM support resulted in shorter LOS when compared to both historic and concurrent control groups. Readmissions were also lower in the intervention cohort as compared to the concurrent control. Due to improved hospital throughput and patient flow practices, this unit received an increased number of ICU transfers. The significant improvement in LOS on this unit has led to expansion of geographic cohorting and multidisciplinary rounds to resident teaching teams as well as other units in our health system.