Background: Hospital at Home (HaH) programs provide feasible and effective inpatient-level care in patients’ homes, with interest in this value-based care model increasing substantially as health systems strain to meet capacity and resource demands.1-6 Despite well-documented benefits, adoption of HaH outside of capacity surges remains limited, hindering scalability efforts.7 Furthermore, patient and provider experiences of HaH remain an understudied component of implementation efforts. Accordingly, our objective is to describe the barriers and facilitators to adoption that patients and referring providers experience as part of an early discharge Hospital at Home program.
Methods: HaH was established in December 2020 at the Atrium Health Wake Forest Baptist. In the early supported discharge model of HaH, a patient who is admitted to a hospital is discharged early at the distal end of their stay, reducing the time spent in the hospital setting. Based on pre-determined criteria, patients deemed appropriate for HaH by the discharging provider are transitioned to receive ongoing care in their home environment. Dedicated nurse navigators were involved in educating patients about the program and allow patient input into the decision. We report a retrospective cohort study of barriers and facilitators experienced by HaH patients (n = 104) and referring providers (n = 55) via online surveys.
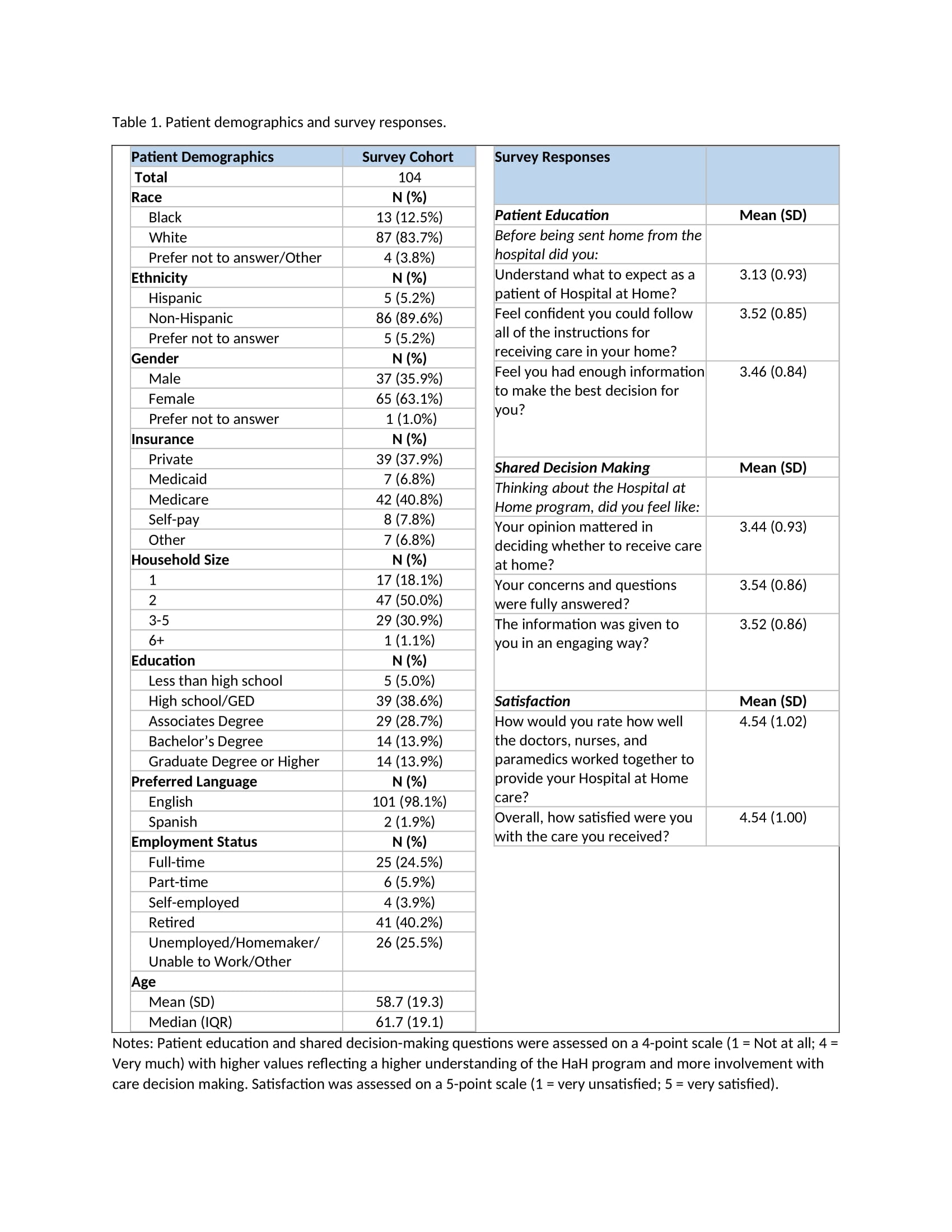
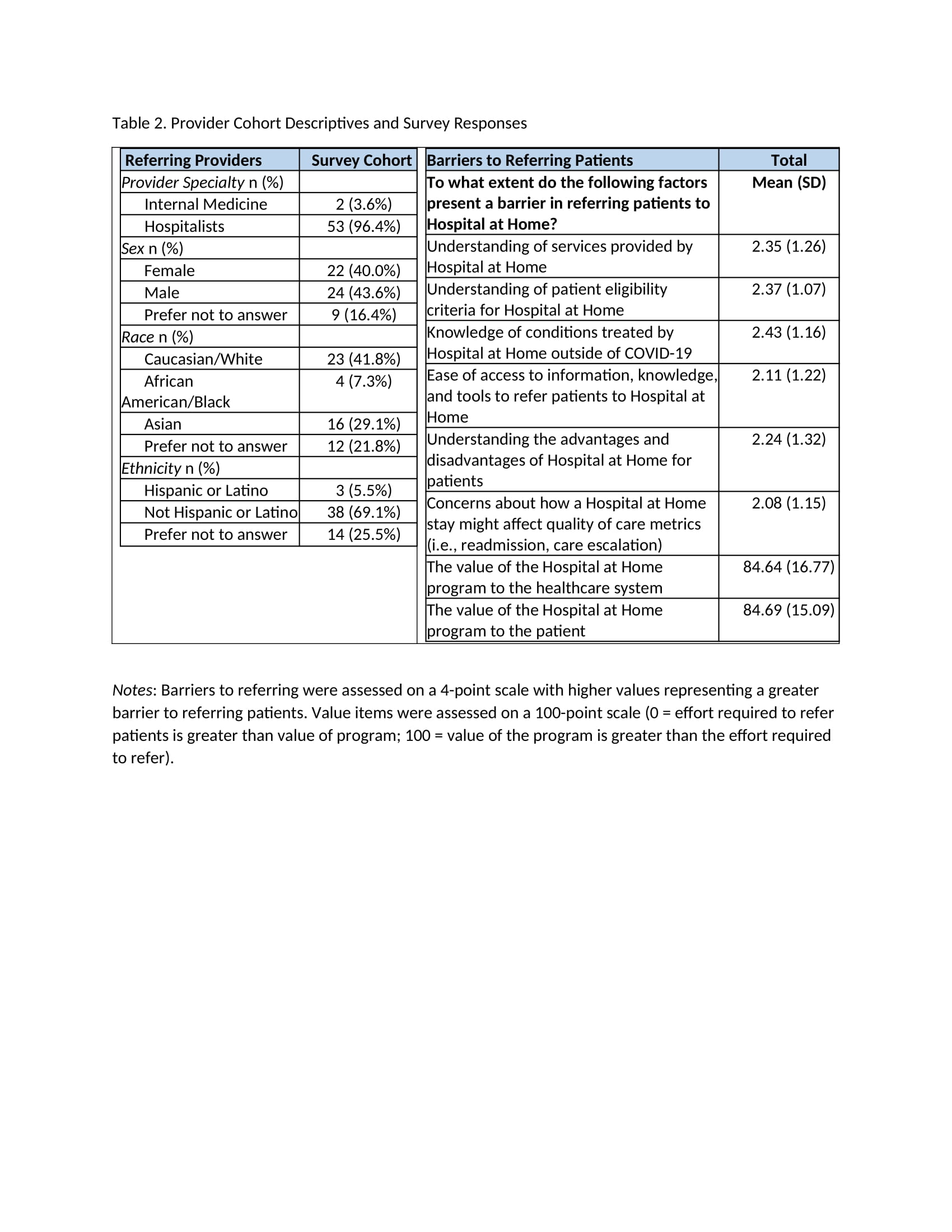
Results: Of the 104 patient survey respondents, approximately 84% identified as White, 13% identified as Black, and 4% preferred not to answer. Most patients were non-Hispanic (89.6%) and beneficiaries of private insurance (37.9%) or Medicare (40.8%). The survey cohort varied in education, employment status, and household size (Table 1). Although there may have been gaps in patient understanding of what to expect from HaH when they agreed to it, they reported high satisfaction with the care they received and the teamwork amongst the members of the HaH team providing the care. This may be, in part, due to the nurse navigator’s involvement in providing easy-to-follow instructions and an opportunity for shared decision-making. Overall, referring providers reported few barriers to referring, including a good understanding of the conditions treated by HaH beyond COVID-19 (Table 2). There was strong consensus on the value of HaH to the patient and health system. Overall, referring providers reported few barriers to referring, with understanding what conditions are treated by H@H beyond COVID-19 (Table 2). There was strong consensus on the value of H@H to the patient and health system.
Conclusions: Utilizing nurse navigators enhanced patient awareness and acceptance of HaH and allowed shared decision-making. Our results suggest that effectively communicating criteria for referrals, including conditions treated, is essential for sustaining continued referrals from providers to HaH.