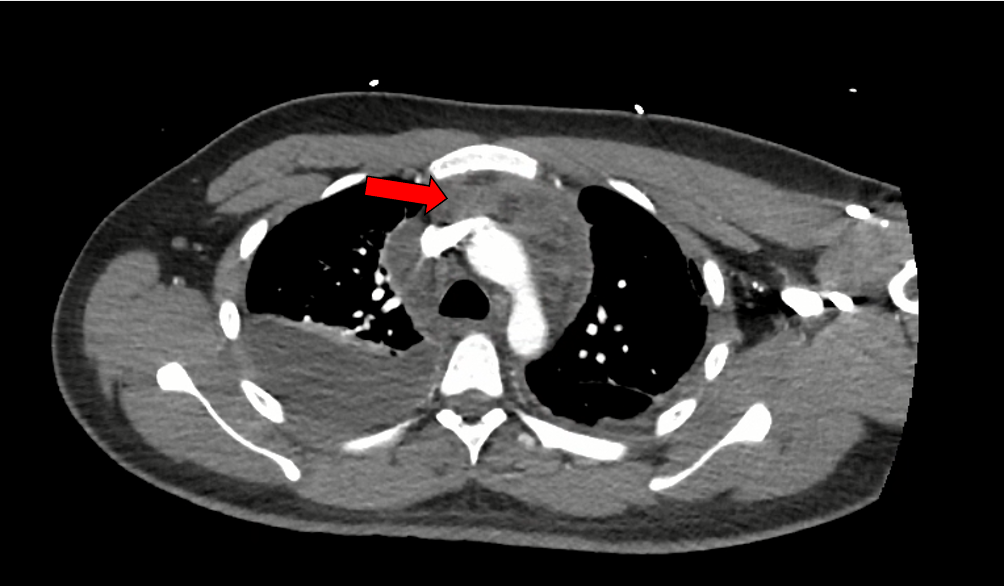
Case Presentation: A 23-year-old male with no significant past medical history presented to an urgent care with six days of fevers, chills, and cough. He was diagnosed with influenza B and discharged home with supportive care. His symptoms continued to progress, and he developed pleuritic chest pain. He presented to the emergency department on day 8 of his illness with a heart rate of 144. A computed tomography (CT) of the pulmonary arteries was negative for pulmonary embolism but showed evidence of pneumonia, bilateral pleural effusions, and a small pericardial effusion. Lab work revealed a mild leukocytosis of 11.79 K/mcL, C-reactive protein 364.3 mg/L, estimated sedimentation rate 42 mm/h, and lactic acid 3.4 mmol/L. Complete metabolic panel, troponin, anti-nuclear antibody, urinalysis, Streptococcus pneumoniae urine antigen, Legionella spp. urine antigen, thyroid stimulating hormone, HIV, group A Streptococcus throat culture, and sputum cultures were unremarkable. He was initially started on vancomycin, ceftriaxone, and three days of azithromycin for treatment of pneumonia, colchicine for pericarditis, and five days of oseltamivir for influenza infection. MRSA probe was negative, so vancomycin was discontinued. Blood cultures returned with one of two positive for methicillin-susceptible Staphylococcus aureus (MSSA). He underwent bilateral thoracenteses with fluid analysis revealing exudative effusions. On day seven of his hospital stay, the ceftriaxone was transitioned to cefazolin 2 g IV every 8 hours. A repeat CT chest was ordered due to the patient’s continued chest pain and it showed a confluent, homogenous mass in the anterior mediastinum consistent with an abscess. Percutaneous biopsy of the mediastinal mass grew MSSA on culture. On day 10, a repeat CT showed partial improvement in the mediastinal abscess size, so the decision was made not to proceed with surgical washout. He was discharged on hospital day 16 on IV cefazolin. Due to the persistent nature of the abscess, cefazolin was continued for a total antibiotic course of eight weeks. After 55 days of therapy, repeat imaging showed resolution of the mediastinal abscess.
Discussion: Influenza is a common viral infection that affects 3 to 11.3% of the U.S. population each year (1). A known complication of influenza is the development of a bacterial coinfection. One study found the prevalence of influenza bacterial coinfection was 20.3%. A common bacterium causing coinfection in this scenario is Staphylococcus aureus (2). Mediastinal abscesses are rare complications that can arise from respiratory infections, with an estimated 4.8 cases per one million people annually (3). Mediastinal abscesses have a mortality rate of up to 40%, so early identification and treatment is imperative (4). Treatment of mediastinal abscesses includes targeted antimicrobials with consideration of more invasive procedures like thoracotomy, video-assisted thoracoscopic surgery, or percutaneous drainage (5).
Conclusions: Influenza infections are common in the United States and can frequently be complicated by bacterial coinfection (2). Mediastinal abscesses are a rare complication that can arise from respiratory infections. This case represents a rare presentation of influenza, Staphylococcus aureus pneumonia, and the development of a mediastinal abscess in a patient with no known risk factors. A review of the literature found one patient case that contained these same elements (6).