Background: Remote patient monitoring (RPM) is a promising new tool to monitor patients who have historically required observation visits in a hospital, or would have remained hospitalized longer if initiated at hospital discharge, and was widely used in the COVID-19 pandemic. We report the outcomes of hospital admission and urgent/emergent care service utilization in a large-scale implementation of COVID-19 RPM (cRPM) as systems, including ours, look to expand RPM beyond COVID-19.
Methods: PDSA of initial protocol development and cRPM roll-out for high risk patients was reported in the journal Chest1. In this updated report, we assess all cRPM admission at Intermountain Health, a large not-for-profit in the intermountain west. Patient encounters across 23 hospitals (i.e., ED discharge and early hospital discharge with cRPM), 24 urgent care centers, and 51 clinics had access to cRPM across Intermountain Health between 8/1/2020 and 12/31/2022. Clinic sites activating cRPM were primarily Obstetrics clinics for monitoring during pregnancy. COVID-19 positive encounters 18 years of age or older were identified, and among these, we assessed encounters in which cRPM was delivered. Basic demographics and data about subsequent visits within a 14-day period to urgent or emergency care, hospitalization, and ICU admission are reported, in addition to 30-day all-cause mortality.
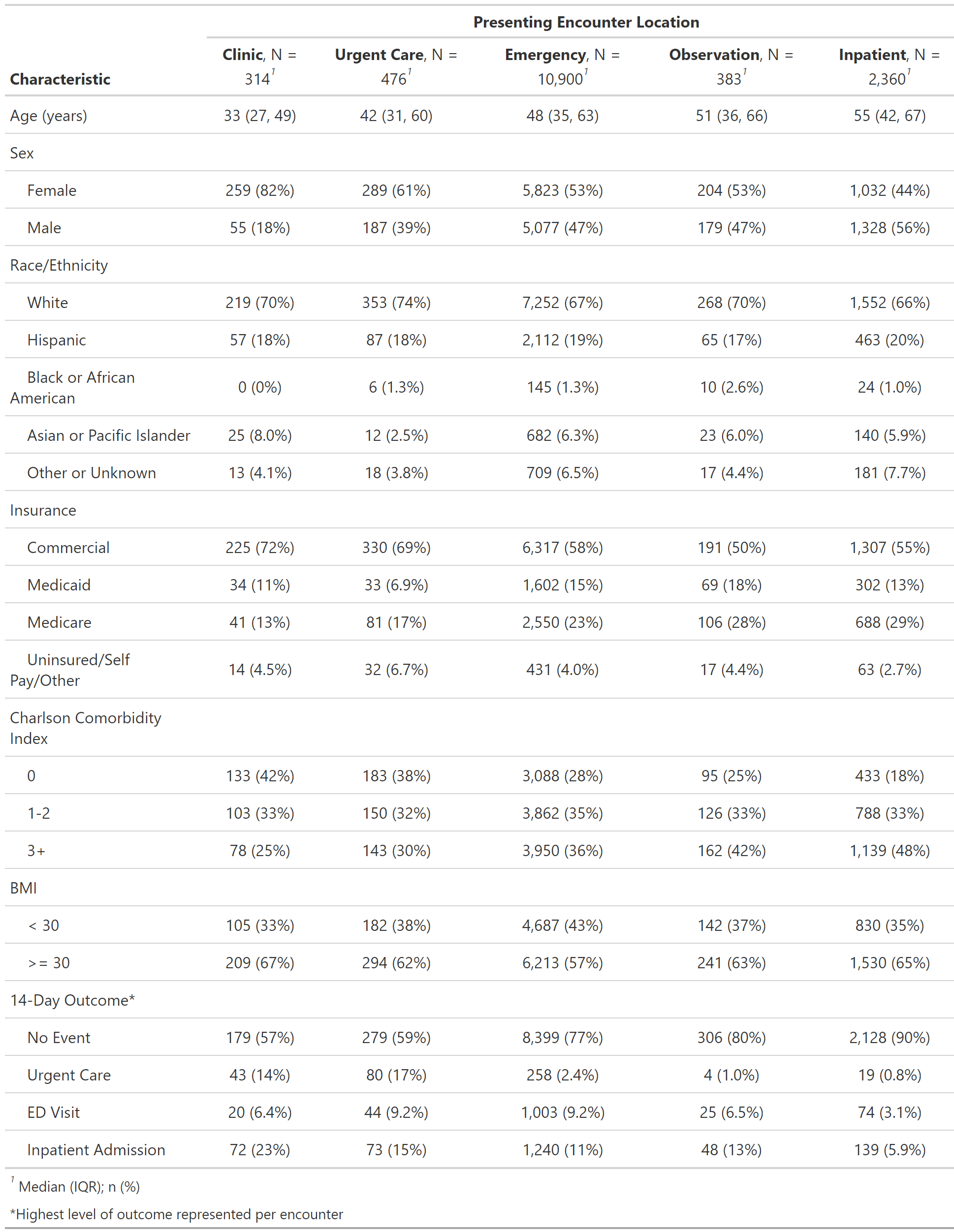
Results: Of the 485,340 COVID-19 encounters assessed across ambulatory, urgent care (UC), emergency department (ED), observation, and inpatient settings, 14,433 encounters (3%) were discharged home with cRPM. The highest proportion of cRPM enrollment was from the ED (n=10,900, 18% of eligible ED COVID-19 encounters). Characteristics of cRPM recipients are summarized in Table 1.Within 14 days of cRPM admission, 18% of patients presented to the ED, 10.89% were hospitalized, and 3% were admitted to the ICU. Overall, the majority of ED visits and hospitalizations occurred between 48 hours and 7 days after starting cRPM. However, patients who received cRPM from urgent care were more likely to represent earlier (13% visited the ED within 48 hours vs 3% between 2-14 days). In contrast, our patients who received cRPM from clinic tended to represent later (2% visited the ED at 48 hours vs 11% between 2-14 days).Overall 30-day all-cause mortality was 0.92%; this was highest (0.96%) among ED cRPM recipients, and lowest (0.32%) among clinic recipients. Similarly, whereas mean LOS among hospitalized patients was 4.88 days (SD 6.07), patients who received cRPM from the ED tended to have longer LOS (5.08 ± 6.23) compared to our clinic population (2.79 ± 4.37).
Conclusions: cRPM is a promising tool to provide appropriate monitoring and care while decreasing utilization of constrained hospital resources. This large-scale deployment during the COVID-19 pandemic provides encouraging results to consider expanding usage of RPM into other settings. How RPM affects resource utilization varies by the clinical setting in which it is deployed.