Background: Efficient discharge planning for hospital medicine patients requires alignment across multiple disciplines. Understanding how clinicians communicate information about discharge readiness can identify opportunities to improve discharge coordination and impact length of stay, hospital capacity, and patient satisfaction. The objective of this study was to outline the existing information gathering and communication pathways around discharge planning across disciplines on our hospital medicine service and identify opportunities to address gaps in communication.
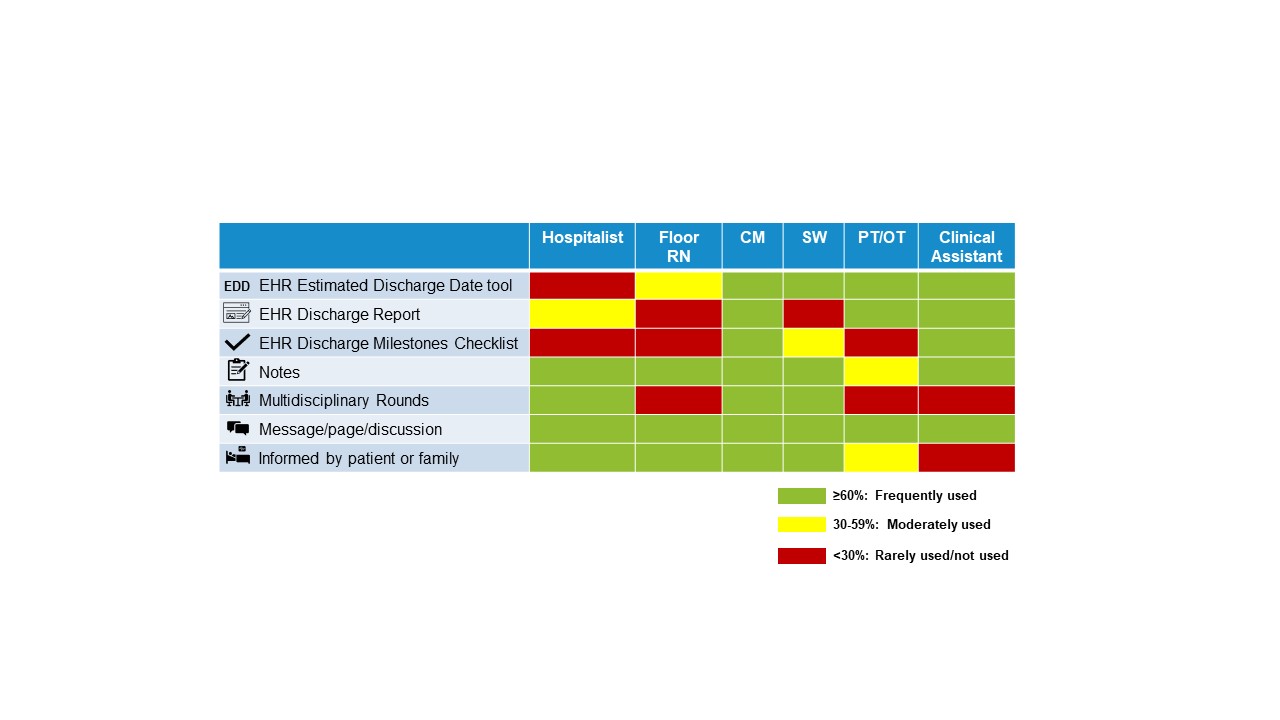
Methods: The study involved multidisciplinary clinicians who participate in discharge planning for patients on the hospital medicine service at a single-site, 800 bed, urban, tertiary care academic medical center. We developed a standardized interview guide based on existing process maps of the hospital discharge planning process with the following 3 goals: 1) understand how clinicians gather and communicate discharge planning information across disciplines, 2) evaluate use of electronic health record (EHR)-based discharge planning tools including Estimated Discharge Date, and 3) identify best practice opportunities for discharge planning communication. We conducted 36 semi-structured interviews (10 hospitalists, 15 nurses, 5 case managers, 3 social workers, 2 physical therapists, and 1 clinical assistant) to generate templated interview summaries from transcripts used to identify key themes. Using this qualitative analysis, we developed process maps for all 6 disciplines interviewed to illustrate discharge planning workflow and tools/approaches used to collect or share discharge planning information from admission to discharge. We used these findings to create a scorecard quantifying how frequently discharge planning tools and communication streams were used by each discipline (Figure 1).
Results: The most common methods used to gather or exchange discharge planning information were written or verbal communication with 94% (34 of 36) of participants using messages, paging, or verbal discussions, 78% (28 of 36) reviewing notes, and 64% (23 of 36) being informed by patients or families. EHR-based discharge communication tools showed variability in usage amongst disciplines. With the estimated discharge date tool, 36% (9 of 25) of hospitalists and nurses reported using the tool while 91% (10 of 11) of the remaining ancillary staff reported using it. Similar trends were observed for the remaining EHR-based tools. Logistical barriers limited multidisciplinary rounds (MDR) participation to physicians, case managers, and social workers. Nurses reported feeling inadequate communication on the discharge plan with the care team with 60% (9 of 15) of nurses reporting scenarios where the patient was the one to inform them on the discharge plan.
Conclusions: We found that most hospital medicine disciplines used written or verbal communication to gather or exchange information to coordinate a discharge. However, ancillary staff, some who do not participate in MDR, were more likely to use EHR-based tools such as Estimated Discharge Date compared to physicians and nurses. Standardizing the source and ensuring the accuracy of information regarding discharge readiness across disciplines in a congruent workflow could help ensure that all clinicians have the information needed to improve discharge efficiency. Our findings demonstrated opportunities to improve discharge planning communication in hospital medicine.