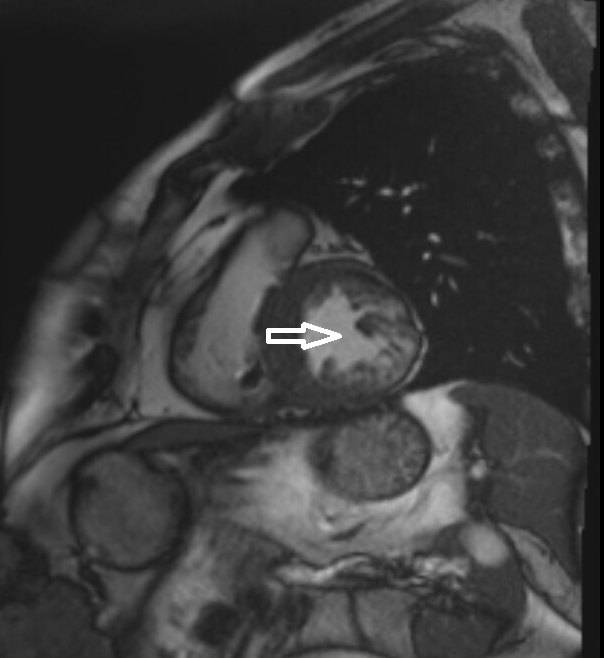
Case Presentation: A 61-year-old male with hypertension, hyperlipidemia, and GERD presented to the ED with intermittent palpitations associated with exertional shortness of breath and near-syncopal episodes since several months. On presentation, he was in sustained Ventricular Tachycardia storm and required defibrillation 5 times despite starting on Lidocaine and Amiodarone infusions along with bolus doses of sotalol. TTE revealed preserved LV function (LVEF 50-55%) with no meaningful valvular disease. Diagnostic testing included left heart catheterization which showed nonocclusive CAD with elevated filling pressures. Diagnostic electrophysiological study indicated an epicardial focus for ventricular tachycardia with initial unsuccessful ablation. He then underwent dual chamber ICD placement. One month later he again presented with an incessant VT resulting in 64 ICD shocks in one day despite bolus amiodarone and lidocaine. He was eventually transferred to a tertiary care center where he underwent successful ventricular tachycardia ablation of epicardial inferolateral scar and right papillary muscle. Cardiac MRI (CMR) showed LVEF 36%, marked hypertrophy of the septum (20 mm) and extensive noncompaction with aneurysm formation most notably involving a large segment of the lateral wall of left ventricle. Diagnosis of left ventricular non-compaction cardiomyopathy (LVNC) was made. Post medical management with ARNI, beta blocker and Spironolactone, patient showed symptomatic improvement at his 1 month follow up.
Discussion: LVNC is a rare congenital disorder. It is characterized by compacted epicardial layer and non-compacted endocardial layer with prominent trabeculations and inter-trabecular recesses which communicate with the left ventricular cavity (1). Most involved segments are the apex, mid-inferior and lateral walls of left ventricle. It usually follows male predominance, occurs in isolation, or associated with other cardiac pathologies. Sarcomere gene mutations are typically involved. Clinical presentation can be varied from being asymptomatic with more severe cases presenting as a triad of heart failure, ventricular arrhythmias, and embolic events. Diagnosis of LVNC can be made via echocardiography, computed tomography (CT), contrast ventriculography, and magnetic resonance imaging (MRI) (2). Accepted diagnostic criteria by Jenni et al. includes (a) Absence of coexisting cardiac abnormalities. (b) Segmental thickening of myocardial wall of left ventricle with two layers: a thin epicardial layer and a thick endocardial layer with prominent trabeculations and deep recesses. The ratio of non-compacted myocardium to compact myocardium at the end of systole is > 2:1. (c) The trabeculae are usually located on the apical/lateral, middle/bottom walls of the left ventricle. (d) The flow between the intertrabecular recesses can be identified by using the color Doppler method (3,4). Treatment includes managing congestive heart failure, antiarrhythmic therapy and in certain cases anticoagulation due to risk of embolic events. The prognosis depends on the degree of heart failure, arrhythmias and associated thromboembolic events.
Conclusions: Hospitalists should be aware of LVNC as a cause of heart failure. This case highlights the importance of using appropriate imaging modalities to prevent delay in diagnosis and management.