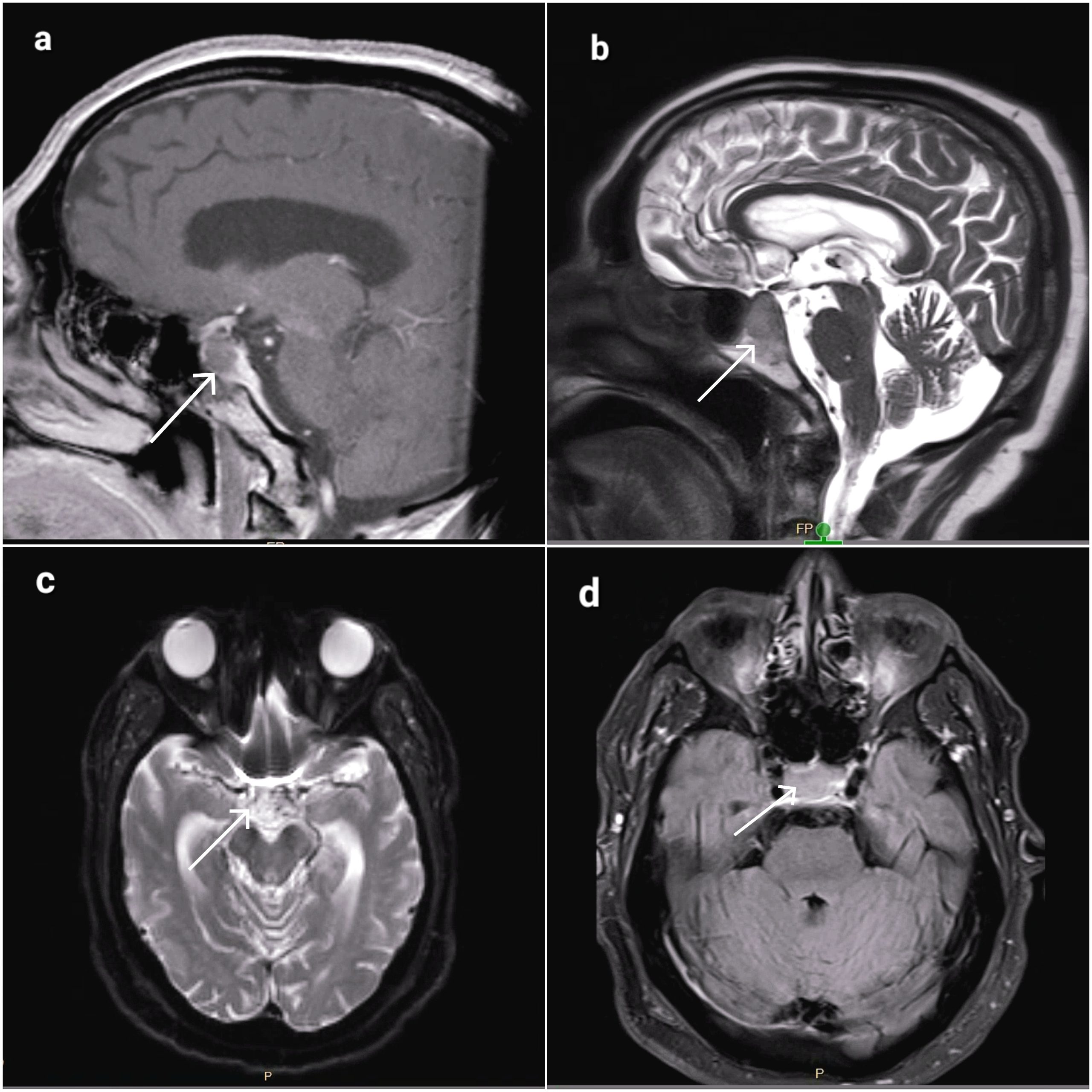
Case Presentation: An 86-year-old male patient with a history of hypertension and newly diagnosed stage 2 prostate cancer was referred from the cancer center due to a hypertensive emergency following the administration of a leuprolide injection. Shortly after receiving the first leuprolide injection, the patient experienced facial flushing, ocular pain, a sensation of eyes bulging out, and dizziness. His systolic blood pressure was above 200 mmHg at the cancer center, unresponsive to antihypertensive medications. He became delirious, which resolved upon reaching the emergency room. The patient denied chest pain, shortness of breath, palpitations, urticarial rash, or tongue swelling. Physical examination revealed subconjunctival hemorrhages, and neurological examination did not reveal any focal abnormalities. An emergency CT scan performed in the emergency department incidentally revealed a pituitary mass measuring approximately 1.5 x 2.0 x 1.2 cm with suprasellar extension, approaching the optic pathway. The sellar floor exhibited erosion, suggestive of tumor extension into the clivus. Of note, the patient did not have any prior diagnosis of pituitary mass/adenoma. MRI with pituitary protocol demonstrated nonenhancement of the mass, raising the suspicion of non-hemorrhagic apoplexy (Figure 1). He also experienced a seizure episode with right gaze preference and jerking of the right arm, and antiepileptic drugs were started. During the hospital stay, he developed a fever of 103°F with confusion. Although no clinical signs of meningitis were evident, empiric treatment for meningoencephalitis was initiated, and he was intubated for airway protection. Vasopressor support and stress-dose steroids were administered for persistent hypotension, but the patient remained hypotensive persistently without multiple vasopressor support, and the patient experienced cardiac arrest and couldn’t be resuscitated. Surprisingly, autopsy revealed macroscopic findings of a 1.4 cm mass within the sella turcica, associated with posterior (clivus) bone erosion, replacing the majority of the normal pituitary gland, exhibiting marked softening, and extensive hemorrhage. Microscopic examination confirmed the presence of a hemorrhagic infarct, confirming hemorrhagic pituitary apoplexy as the cause of death.
Discussion: Leuprolide binds to GnRH receptors and downregulates the production of FSH and LH, leading to a reduction in testicular and ovarian steroidogenesis. Theoretically, leuprolide can stimulate and increase metabolic activity in the underlying pituitary adenoma. This surge may surpass the adenoma’s blood supply, causing ischemic necrosis and hemorrhage. Our patient presented with apoplexy minutes after the first injection of leuprolide administered in the cancer center, despite having no prior diagnosis of a pituitary adenoma.
Conclusions: It is important for physicians to recognize the rare but life-threatening association between the use of GnRH analogs and pituitary apoplexy. Hence, pituitary adenoma should be excluded in patients being started on leuprolide for prostate cancer. It should be considered as a differential when patients taking leuprolide experience headaches and unexplained neurological symptoms.