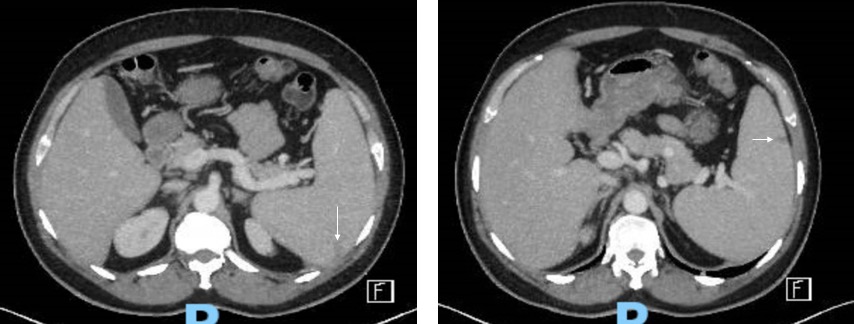
Case Presentation: We present a case of a 49-year-old male with a history of hereditary thrombocytosis who presented to the Emergency Department with a 4-day history of intermittent fevers, headache, nausea, abdominal pain and one episode of emesis. The patient recently returned from travel to Yemen. He was not taking anti-malarial prophylaxis. Initial vital signs were a temperature of 38.3C, heart rate of 99 beats per minute, blood pressure 138/78 mmHg and respiratory rate of 20 breaths per minute. Laboratory data revealed leukopenia of 2610/uL, hemoglobin of 11.8 g/dL, platelet count of 354,000/uL, AST 113 iU/L, ALT 197 iU/L, total bilirubin 1.0 mg/dL, CRP 145.3 mg/L, LDH 550 U/L, and procalcitonin 0.58 ng/mL. Historically, his baseline platelet count was ~1,000,000/uL. He received empiric broad-spectrum antibiotics with vancomycin and piperacillin-tazobactam for suspected sepsis, although without a clear source. Given the report of recent travel, the diagnostic evaluation was broadened to include travel-associated infections.To further evaluate the abdominal pain, computed tomography of the abdomen and pelvis was performed (Figure 1), and was notable for splenomegaly with wedge-shaped hypodensities concerning for splenic infarcts. Urine and bacterial blood cultures showed no growth. Serologies for EBV, CMV, and Toxoplasma were suggestive of past infections. Hepatitis panel and legionella urinary antigen were negative. Ehrlichia, Anaplasma, Rocky Mountain Spotted Fever, and Dengue serologies were negative. A transthoracic echocardiogram revealed normal left ventricular function and showed no valvular abnormalities. A blood smear revealed Plasmodium falciparum by Giemsa stain with parasitemia of 1.2%. The patient completed a course 3 day course of atovaquone/proguanil. Repeat parasitemia smears showed no evidence of blood parasites, and liver enzymes began to decrease. He was discharged home on hospital day 6.
Discussion: Infarctions of the spleen may present in a variety of medical conditions and likely portend an underlying alternative diagnosis. The most common conditions where splenic infarctions are seen are thromboembolic and infiltrative hematologic diseases [1].Even with prophylactic medications, malaria poses a significant risk to travelers and those in endemic areas. A recognized sequela of malarial diseases is splenomegaly, and rarely splenic infarctions have been reported [2-3]. In the literature Plasmodium vivax is the Plasmodium spc. reported as the largest precipitant of splenic infarcts [2]. Outcomes of splenic infarction in Plasmodium infections remain favorable with conservative measures (i.e. appropriate anti-malarial treatment and pain control) [2-3].
Conclusions: Splenic infarctions are present in the background of a variety of clinical diseases. Splenomegaly is a recognized complication of malarial illness, however, splenic infarctions are rare and likely underreported. Splenic infarction should be kept in the differential when evaluating a patient presenting with abdominal pain and recent travel history to malarial endemic nations.