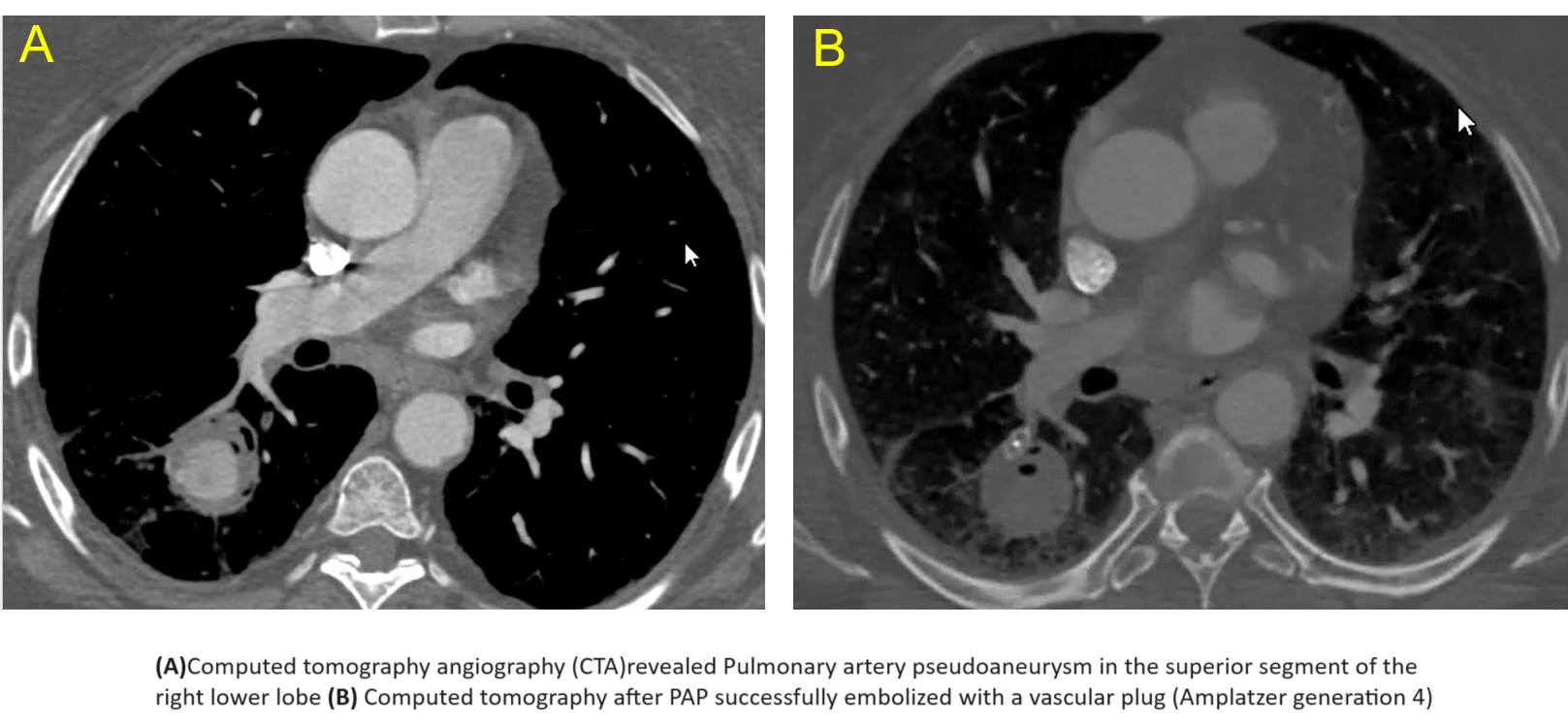
Case Presentation: A 65-year-old obese woman with type II diabetes mellitus presented with a 7-day history of cough and hemoptysis described as streaks of blood during the first two days, and as half a cup to a cup of bright red blood with clots thereafter. On arrival to the emergency room she was hemodynamically stable, in no respiratory distress, and her SpO2 on room air was 98%. Hb was 11 g/dL (five weeks earlier it was 15 g/dL). She denied any history of pulmonary injury. Seven weeks earlier she was hospitalized with COVID-19 pneumonia for which she received supplemental oxygen with high flow nasal cannula, remdesivir, dexamethasone and tocilizumab. On current admission, computed tomography angiography revealed a Pulmonary artery pseudoaneurysm (PAP) in the superior segment of the right lower lobe. (Chest radiograph obtained seven weeks earlier revealed normal pulmonary vasculature and no nodules. A non-contrast computed tomography obtained approximately six years earlier revealed normal caliber central pulmonary arteries and no nodules.) The PAP was successfully embolized with a vascular plug (Amplatzer generation 4). During hospitalization the patient underwent transesophageal echocardiogram which was negative for vegetations. Fungal and bacterial blood cultures and viral panel were all negative. Recovery was successful with no recurrence of hemoptysis.
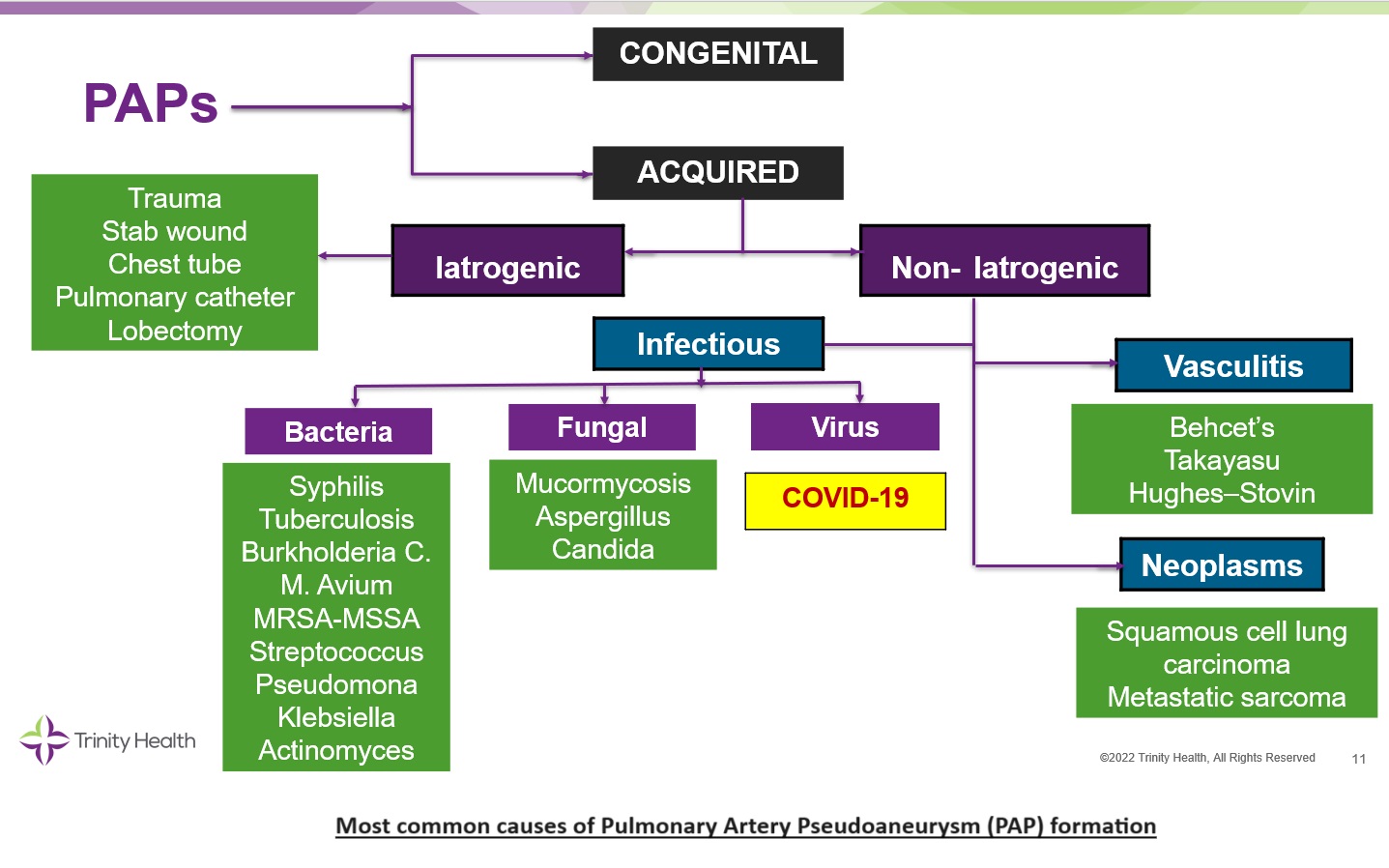
Discussion: Pulmonary artery pseudoaneurysms (PAPs) result from a focal dilatation of a segment of pulmonary artery which histologically involves only the outer layers of the arterial wall (media and adventitia). PAPs can be congenital. In our patient, however, imaging antedating her hospitalization was negative for PAP signifying that her PAP was acquired. Our patient had no history of iatrogenic or non-iatrogenic trauma, vasculitis or bacterial or mycotic infection. Accordingly, we reason that her PAP was most likely triggered by the earlier episode of COVID-19 pneumonia. Post-COVID-19 PAP is an exceedingly rare complication so far reported in a handful of patients. SARS-CoV2, the virus responsible for COVID-19, is known to cause diffuse alveolar damage and associated vasculopathy. Whether vasculopathy caused by SARS-CoV2 infection is the mechanism at play in the development of post-COVID-19 PAP remains to be determined. Clinically, PAP can cause no symptoms, or it can cause cough, and hemoptysis. The latter can be massive with a mortality rate exceeding 50%.
Conclusions: Our case illustrates a patient with acquired PAP diagnosed seven weeks following COVID-19 pneumonia which was successfully embolized. Rare cases of PAP-associated with COVID-19 have been reported in the literature. Accordingly, the differential diagnosis of a new lung nodule/focal consolidation following COVID-19 pneumonia–whether the patient is symptomatic or not—must include development of an [[[acquired]]] PAP. Identifying this serious complication is critical for the institution of appropriate therapy to prevent life-threatening hemoptysis. In addition, this case will also bring awareness of the variety of presentations and complications related to COVID-19 infection.