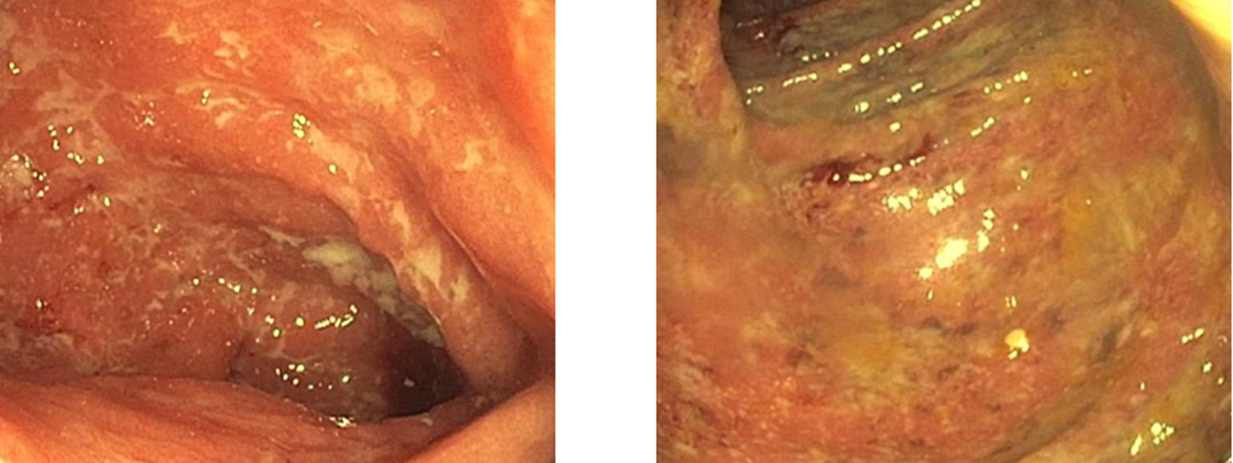
Case Presentation: A 29-year-old male with a past medical history of uncomplicated bio-naïve mild ulcerative colitis (UC) diagnosed on a recent colonoscopy on oral mesalamine 4.8 grams/day presented to the hospital for acute onset central chest pain two weeks after initiation of therapy. The character of the chest pain was sharp, worsening with deep inspiration, and improving when leaning forward. On physical exam, the patient was vitally stable but tachycardic, with a heart rate of 115 beats per minute. His heart sounds were regular in rhythm, with a normal S1 and S2 and no murmurs, rubs, or gallops. Laboratory examination reported mild leukocytosis 13,970/µL, microcytic hypochromic anemia 10.3 g/dl, and thrombocytosis 457,000/µL. The comprehensive metabolic panel was unremarkable. C-reactive protein (CRP) was increased to 159.8 mg/L, NT-ProBNP was increased to 900 pg/mL, high-sensitivity troponin level was increased to 90 ng/L, and D-dimer was increased to 2.01 ug/mL. Computed Tomography (CT) angiography did not report a pulmonary embolism. An electrocardiogram (EKG) showed sinus tachycardia, PR segment depression, and ST-segment elevation in the inferolateral leads. An echocardiogram showed normal morphology of the left and right ventricles, a left ventricular ejection fraction of 55%, mild mitral regurgitation, and no signs of pericardial effusion. The patient’s clinical presentation was consistent with acute pericarditis, presumed to be secondary to the recent initiation of oral mesalamine. Mesalamine was stopped, and the patient was started on prednisone 30 mg daily and colchicine 0.6 mg daily. The patient responded well to treatment and was thus discharged with prednisone 30 mg daily with a plan to taper by 10 mg every week and colchicine 0.6 mg daily for one month. At a follow-up gastroenterology visit, the patient was started on Ustekinumab to treat UC. Both steroids and colchicine were discontinued entirely. At the latest follow-up visit, the patient continues to be in clinical remission for UC without any further episodes of chest pain or hospitalizations for acute pericarditis.
Discussion: Multiple immune-mediated inflammatory diseases, including inflammatory bowel diseases (IBD), are associated with a higher risk of myocarditis and pericarditis. Nevertheless, the risk of myocarditis in IBD is low [8.3 per 100 000 patient-years in CD; 2.6 per 100 000 patient-years in UC]. Medications used in the treatment of IBD have also been associated with myocarditis. These include mesalamine and tumor necrosis factor alpha (TNFa) antagonists. It remains a challenge to determine whether the risk is driven by medications or IBD itself. Pericarditis is also more likely to affect IBD patients compared to population controls. Unlike myocarditis, pericarditis is almost always driven by medications, with complete resolution after treatment withdrawal. In our case, the patient’s symptoms started two weeks after the initiation of mesalamine therapy and resolved soon after its discontinuation. Early diagnosis and proper patient education are essential.
Conclusions: The major challenge in managing these patients is the need for a high index of suspicion for medication-related side effects in IBD patients on anti-TNF medications and 5-ASA derivatives presenting with acute chest pain. Timely discontinuation of mesalamine results in favorable outcomes. Early diagnosis and proper patient education are crucial.