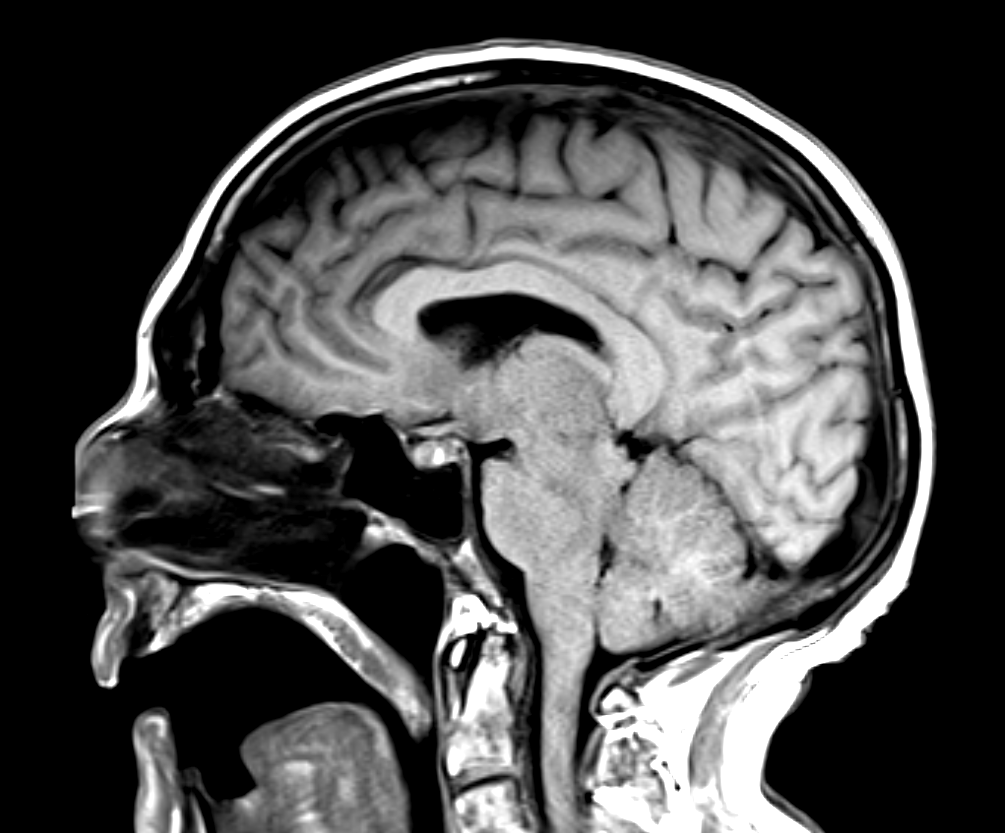
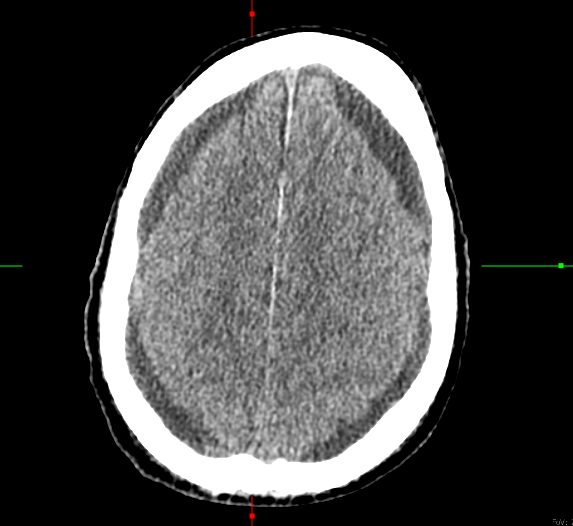
Case Presentation: A 65-year-old male presented to his primary care clinic with a one-week history of right-sided facial pain radiating around his jaw with a negative dental workup. Patient had progressive neck pain and CT scan found an ill-defined soft tissue in the superior mediastinum encasing the proximal left common carotid artery, concerning for lymphoproliferative disease. Laboratory workup revealed a significant leukocytosis, suggesting possible hematologic malignancy or acute infection with leukocytosis of 35.3 with left shift and mild thrombocytopenia. The patient’s workup revealed High Grade B-Cell Lymphoma with central nervous system (CNS) involvement. Bone marrow biopsy revealed hypercellular marrow with 100% involvement by CD10+ large B cells. FISH showed t(8,14), which is consistent with Burkitt’s Lymphoma. The patient was admitted to the Hematology Oncology service and started cycle 1 treatment with dose-adjusted rituximab, etoposide, prednisolone, vincristine, cyclophosphamide, doxorubicin IV, and intrathecal (IT) methotrexate (MTX). This cycle of chemotherapy was complicated by septic shock secondary to invasive pulmonary aspergillosis and diffuse alveolar hemorrhage, as well as severe headaches and hypersomnolence. The MRI of the brain revealed subacute cerebellar and acute occipital infarcts without evidence of small vessel disease, as well as trace bilateral subdural fluid collections. The patient’s somnolence improved and he started cycle 2 of chemotherapy where he began to have somnolence and potential seizure-like activity again. Repeat CT head noted increasing subdural hygromas to 5mm, evolving occipital stroke with hemorrhagic features, and descending midline herniation with compression on the brainstem; Neurosurgery and Neurology were consulted. The cause of his midline herniation was proposed to be from increasing subdural hygromas and intracranial hypotension from cerebrospinal fluid (CSF) leak associated with lumbar punctures. A CSF blood patch was recommended.Overnight, the patient decompensated and developed acute hypoxic respiratory failure and worsening mental status, and the family pursued comfort care measures.
Discussion: Subdural hygromas affect approximately 1% of patients receiving IT MTX, however, there is a dearth of literature outlining subsequent CSF leak with transtentorial herniation and intracranial hypotension–which, in this case, resulted in a fatal complication. Patients may be asymptomatic, but symptoms such as headache, and worsening somnolence may serve as a warning sign [1,3,4]. The pathophysiology of subdural hygroma formation remains unclear, and the proposed mechanisms are multifaceted. Hypotension, decreased intracranial pressure, and CSF leak are presumed to be involved, which this patient’s clinical course was consistent with. Downward displacement of the brain may facilitate CSF accumulation in the subdural space due to disruption of the arachnoid granulations which are responsible for CSF absorption [2-4].
Conclusions: Bilateral subdural hygromas, followed by CSF fluid leak and transtentorial herniation, are a rare complication of IT MTX therapy which may be a challenge to recognize and promptly attempt treatment. As highlighted in this case, the constellation of certain clinical and neurological symptoms may alert clinicians to further work up patients receiving IT MTX chemotherapy for potential subdural hygromas and CSF fluid leak.