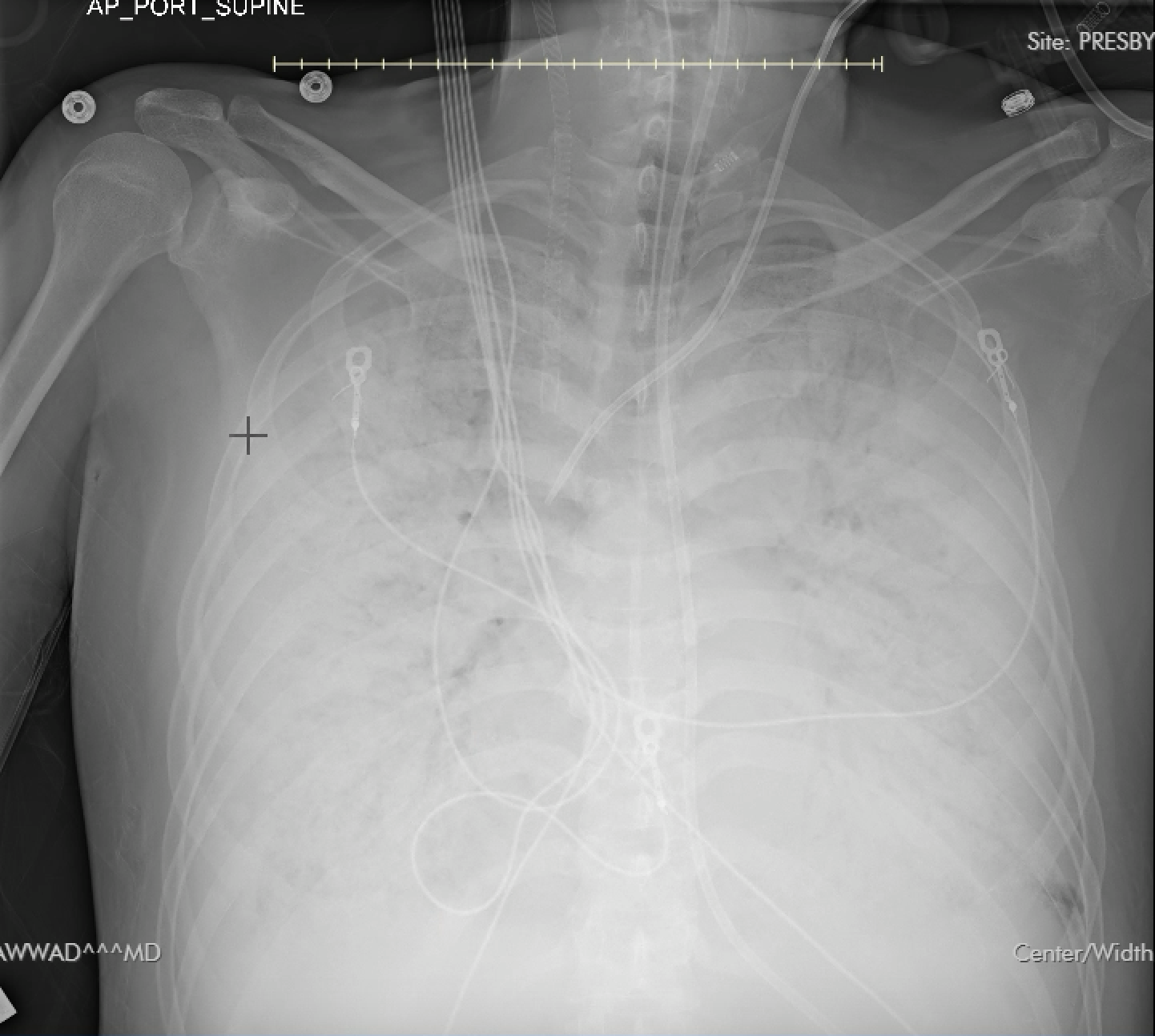
Case Presentation: A 53-year-old Vietnamese monk living in a rural Texas monastery presented with fatigue, muscle aches, and fever that progressed to respiratory distress after a two-week delay in seeking care. He was intubated and sedated at a tertiary care center. He was afebrile, tachycardic (HR 122 bpm), and normotensive. Labs showed a leukocytosis (WBC 22.5k), creatinine 1.29, troponin 0.127, and platelets 217k Imaging revealed diffuse bilateral pulmonary opacities and lower lobe edema. Chest X-ray revealed infiltrates suspicious for pulmonary edema. The differential diagnosis included community-acquired pneumonia and an unlikely differential of Hantavirus Pulmonary Syndrome (HPS), given that he lived in a rural monastery with outside grain storage. It was later determined that another monk in the monastery had died from similar symptoms. The patient was treated with broad-spectrum antibiotics and started on assist-control ventilation (FiO2 100%, PEEP 14). Worsening hypoxia resulted in the use of pressure control ventilation with high PEEP, proning, and paralysis. He continued to decline and remained hypoxic on maximal ventilator settings. On day 7, venous-venous (VV) ECMO was initiated due to hypoxemic respiratory failure. Echocardiography revealed severe mitral regurgitation with posterior leaflet prolapse, requiring LV offloading with an LVAD. Due to concern for lack of improvement on steroids and antibiotics, hantavirus serology was sent. He developed a worsening leukocytosis (20.56k), thrombocytopenia (33k), coagulopathy (aPTT of 110.7), and shock liver (AST 1,112, ALT 478). Labs also showed severe metabolic acidosis (pH 6.97). Repeat Chest X-ray showed ARDS. Hantavirus IgM confirmed HPS on day 14. Despite transient improvement, the patient required multiple vasopressors and progressed to multi-organ failure. The family opted for comfort measures, and care was withdrawn.
Discussion: HPS is a rare, severe disease causing increased pulmonary capillary permeability, edema, and respiratory failure. Mortality reaches 40%, with cases in the U.S. linked to deer mouse exposure. There have been 846 recorded cases of HPS in the US since 1993. Prevention involves pest control and public education on rodent avoidance. This case parallels a report of a 22-year-old male with similar symptoms. In both, ECMO was required, but the younger patient had early VA ECMO secondary to cardiogenic shock, while VV ECMO was delayed until day 7 here for hypoxemia. The use of early ECMO may improve outcomes due to decreased mortality if the patient survives the cardiopulmonary phase of the disease. Delayed presentation, severe infection, and older age likely contributed to this patient’s poor outcome. Management of HPS is primarily supportive, with no proven benefit from glucocorticoids or Ribavirin. Early recognition and intervention are critical for survival. Public health advisories in rural areas can help reduce delayed presentations by promoting early medical attention in high-risk settings.
Conclusions: This case highlights the diagnostic and management challenges of HPS, particularly with delayed presentation. Preventive strategies and early interventions are essential to improve outcomes in high-risk populations.