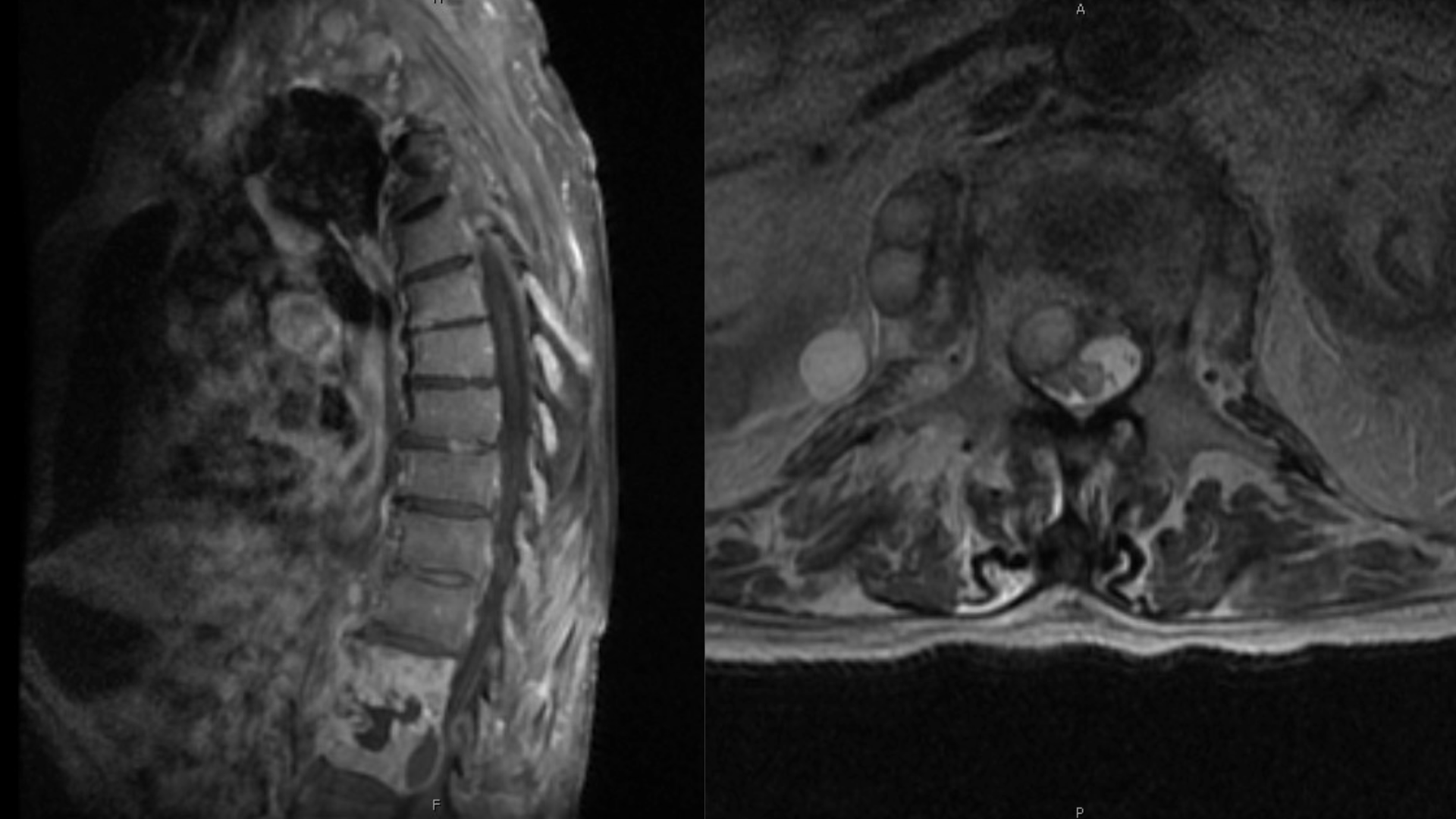
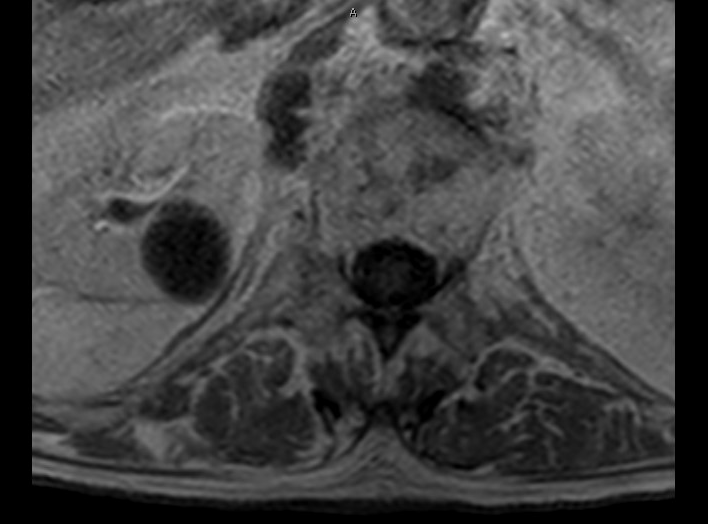
Case Presentation: An 86-year-old male with a past medical history of bladder cancer, status post Bacillus Calmette-Guerin (BCG) therapy 12 months prior, presented to the ED with three months of progressively worsening back pain and weight loss. He denied cough, fever, night sweats, dysuria, recent travel, history of farming, exposure to cattle, or consumption of unpasteurized dairy products. On examination, he was hypertensive, afebrile, and found to have limited ROM of the lumbar spine and no focal neurological deficits. Laboratory studies revealed creatinine 1.4, ESR 62. An MRI lumbar spine demonstrated: T12-L1 discitis-osteomyelitis; a 2.5cmx1.3×1.0 cm anterior epidural abscess at L1; and a 2.9 x 2.7 x 1.3 cm right psoas abscess adjacent to T12-L1. The patient was started on broad-spectrum IV antibiotics; he did not meet surgical indications. During the hospitalization, blood cultures were negative. The patient was transferred to a tertiary care facility for further management. A biopsy of the right psoas abscess revealed Mycobacterium bovis. Preliminary results for acid-fast bacilli on sputum culture were negative. The patient was started on rifampin, isoniazid and ethambutol and continues to be monitored.
Discussion: Bacillus Calmette-Guérin (BCG) is a live-attenuated strain of Mycobacterium bovis used for intravesical immunotherapy for bladder cancer. BCG infection itself is rare (118 cases from 2004-2015) and infectious complications occur in less than 5% of treated patients [1]. The pathogenesis of disseminated M. bovis is thought to be secondary to systemic mycobacterial infection and local inflammatory hypersensitivity at various sites. Infectious complications of intravesical BCG therapy are rare and more common in the immunocompromised. Additional risk factors include age >70, traumatic catheterization, acute cystitis and persistent gross hematuria after transurethral surgery [2]. Direct transmission of M. bovis is rare but possible and is seen in farmers who work with cattle or through the consumption of unpasteurized dairy [3]. Musculoskeletal complications of intravesical BCG therapy are rare. To the best of our knowledge, there have been only 6 reported cases of M. bovis epidural abscess following BCG therapy in the past 50 years. Osteomyelitis, spondylitis, epidural and psoas abscesses are rare musculoskeletal complications [4]. Clinical manifestations of disseminated musculoskeletal disease include fever, night sweats, weight loss, pain, and possible focal neurological deficits [5]. MRI is the best imaging modality for detecting discitis-osteomyelitis and spinal/intramuscular abscesses [6]. The gold standard for diagnosis of M. bovis infection is mycobacterial culture with speciation confirmed by PCR [7]. Treatment of M. bovis consists of rifampin, isoniazid, and ethambutol for approximately 9-12 months. Treatment does not typically include pyrazinamide, since resistance is very common [8]. Timely initiation of treatment is associated with more favorable outcomes [9]. Potential long-term sequelae include vertebral compression fractures, neurologic deficits and chronic pain. Due to the paucity of reported cases, mortality is unknown [10].
Conclusions: Physicians should consider Mycobacterium bovis in patients who present with infectious manifestations in the setting of previous BCG therapy.