Background:
Neutropenia is a serious and potentially fatal complication of drug therapy that can be induced by a number of medications. Failure to correctly identify and remove the offending agent can result in serious morbidity and mortality.
Methods:
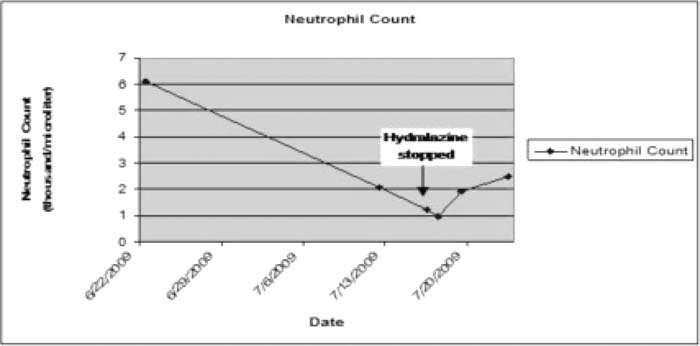
The patient is a 52‐year‐old African American woman with diabetes, chronic anemia, and refractory HTN who presented with shortness of breath and was found to have a decreased WBC count and low platelets. Admission WBC count was 2.3 × 103/μL, with a neutrophil count of 1.24, platelets 155, and hematocrit at baseline of 26. By hospital day 2, ANC decreased to 960 and platelets to 127,000/μL. Review of her medication regimen revealed That she was taking aspirin, fluoxetine, glipizide, gabapentin, HCTZ, metoprolol, nifedipine, rosuvastatin, pantoprazole, and hydralazine. Hydralazine 150 mg daily had been started 36 days earlier. Laboratory analysis revealed weakly positive ANA; however, anli‐double‐stranded DNA, antihistone, and anti‐RNP antibodies were negative. Lupus inhibitor was nondiagnostic. Complement levels were within normal limits. Serum and urine protein electrophoresis revealed no monoclonal spikes. HIV and hepatitis serologies were negative. Drug screen and history were negative for illicit drug or EtOH use. A peripheral smear revealed microcytic anemia and no other abnormalities. Hydralazine was stopped, and after 5 days the WBC count had risen to 3.6 × 103/μL with a neutrophil count of 2.5 × 103/μL and a platelet count of 264,000/μL. No other medication changes were undertaken. In consultation with hematology, it was concluded that her presentation was consistent with hematologic abnormalities due to hydralazine.
Results:
More than 125 different drugs have been reported to cause neutropenia, often through idiosyncratic reactions that are not well understood Mechanisms including either increased peripheral destruction or decreased bone marrow production are believed to be responsible. Agranulocytosis is seen with multiple classes of drugs, with the highest relative risks for analgesic, NSAID, antiarrhythmic, antithyroid, anticonvulsant, cardiovascular, Gl, and antirheumatic medications. Hydralazine has been frequently associated with pancytopenia in the context of full‐blown drug‐induced lupus, but rarely in its absence, as in our patient.
Conclusions:
When unusual clinical presentations appear, iatrogenesis in the form of unusual medication reactions must always be considered, particularly in patients subject to polypharmacy.
Author Disclosure:
A. Melzer, none.