Background: Ten to twenty percent of U.S. hospitalizations are avoidable, driven by clinical uncertainty, social factors, or lack of access to ambulatory care [1-3]. These unnecessary admissions result in significant human and financial costs, including in-hospital errors, wasteful spending, and medical debt [4-7]. With hospital occupancy reaching critical levels, we designed and launched the Olive View-UCLA Next Day Clinic (NDC), an innovative outpatient model offering hospital-level services to divert hospital admissions, thereby addressing overcrowding and improving acute care.
Methods: We report results from the first 13 months (July 2023-July 2024) of NDC operations. The NDC provides high-acuity follow-up appointments within 12 hours for patients referred from the ED who would otherwise be admitted. Patients return daily for services like IV antibiotics, IV diuretics, or imaging studies (e.g., echocardiograms), avoiding hospitalization (Figure 1). Hospitalists approached ED physicians about patients being hospitalized (as evidenced by an InterQual® order) to inquire about NDC referral, at which point ED physicians would agree to divert to NDC versus admit as usual. To estimate hospital bed-days avoided and cost savings, we used a bounding exercise. For the lower (conservative) bound, we assumed that only referrals that met InterQual® criteria avoided hospitalizations. For the upper bound, we assumed 80% of NDC referrals (regardless of InterQual®) avoided hospitalization. We performed propensity score matching of NDC patients with hospitalized counterparts on age, sex, primary diagnosis, and first set of ED labs and vitals to create a control group of inpatients to calculate the difference in days alive and out of hospital (DAOH) at 30 days post-ED visit.
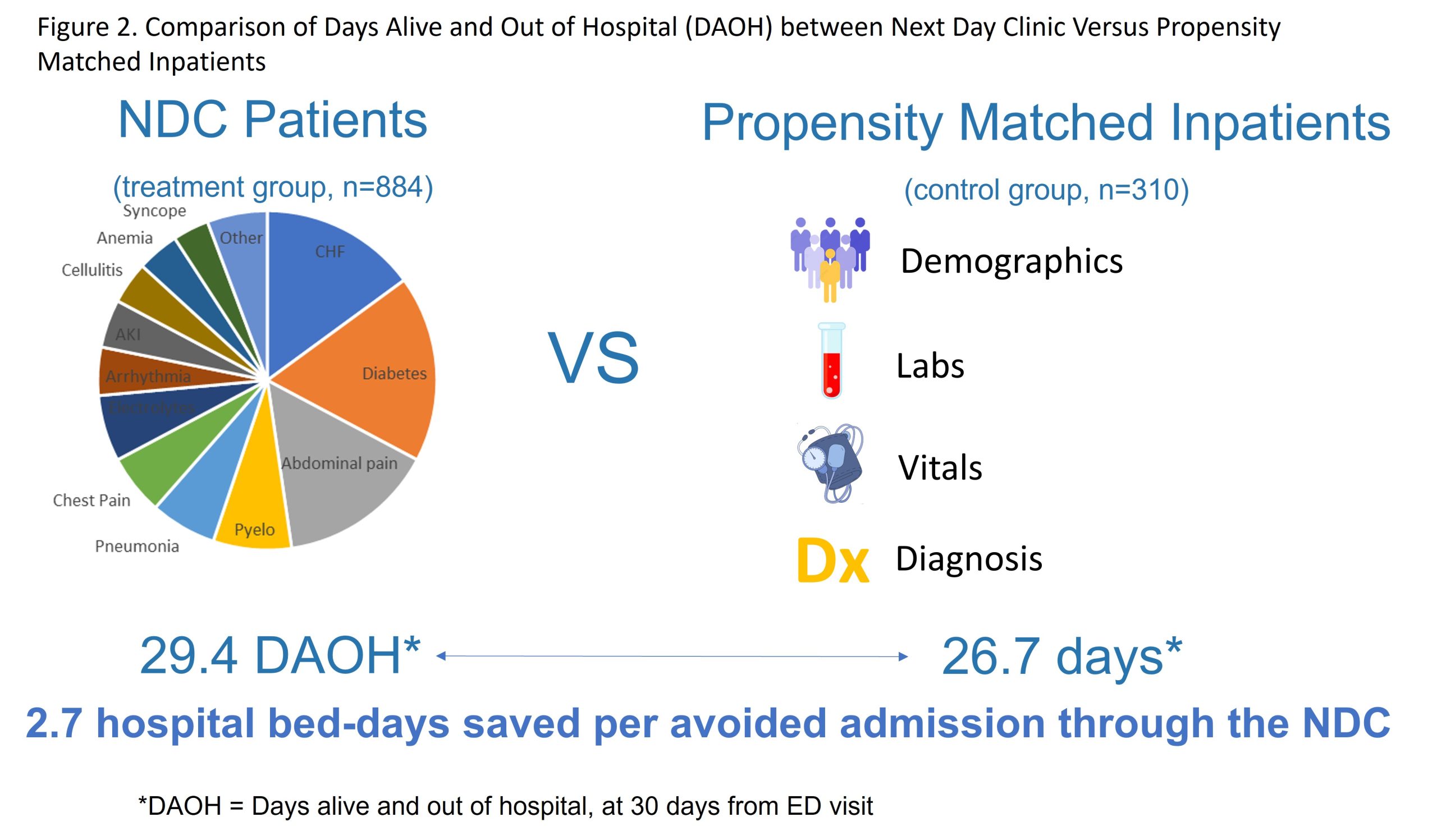
Results: The NDC treated 884 patients (on 1009 referrals; 88% show rate) between July 2023-July 2024. Demographics were: mean age 54 years, 44% female, 77% Hispanic/Latino, 100% Medicaid eligible, 63% Spanish primary language. Of these, 93 (22%) met InterQual® criteria. The DAOH was 29.4 for the NDC group compared to 26.7 for the matched inpatient controls, imputing that each avoided hospitalization saved 2.7 hospital bed-days (Figure 2). The bounding exercise suggested that 93-336 (22-80%) of referrals avoided hospitalizations, which translates to 260-941 hospital bed-days saved. Using actual Medicaid reimbursements for the case-mix of conditions seen in the NDC (average $13,420 per hospitalization; mean LOS 6.1 days; $2,200 per hospital bed-day), the NDC saved $573,000 to $2.07 million in 13 months.
Conclusions: The NDC substantially reduced healthcare expenditures, decreased hospital and ED overcrowding, and maintained high-quality outpatient care within a safety net hospital. This model is highly scalable and low-cost to implement (especially in resource-constrained settings) given that it is co-located with an Urgent Care, and can be used to supplement Hospital at Home or other hospital avoidance models.