Background: Coffee is a widely consumed beverage. Evidence suggests that coffee consumption is associated with a substantially lower risk of type 2 diabetes (1). However, there is paucity of literature on whether coffee consumption has any protective effect on people who already have diabetes. We sought to examine the association between caffeine consumption and hemoglobin A1c (HbA1c) among adults with diabetes in US population.
Methods: We used the data from National Health and Nutrition Examination Survey cycles 6, 7, and 8 (NHANES 2009-2014). Diabetes status was self-reported. Average daily caffeine consumption was calculated based on two 24-hour dietary recall interviews. Each variable was summarized by the mean and standard error for continuous variables and frequency and percent for categorical variables. Baseline patient characteristics were compared by using ANOVA for continuous variables and Chi-squared tests for categorical variables. Univariate and multivariable linear regression modeling was performed for HbA1c as a continuous outcome with average daily caffeine as the primary predictor of interest. Multivariable models were each adjusted for age, gender, race, BMI, income to poverty ratio (IPR), insurance, education, daily physical activity, smoking status, total daily calories, daily fat and magnesium intake, and current diabetes medications. All analyses were adjusted for the NHANES survey sampling design using the appropriate weights. Data processing and analysis were performed using SAS 9.4 (SAS Institute, Cary, NC).
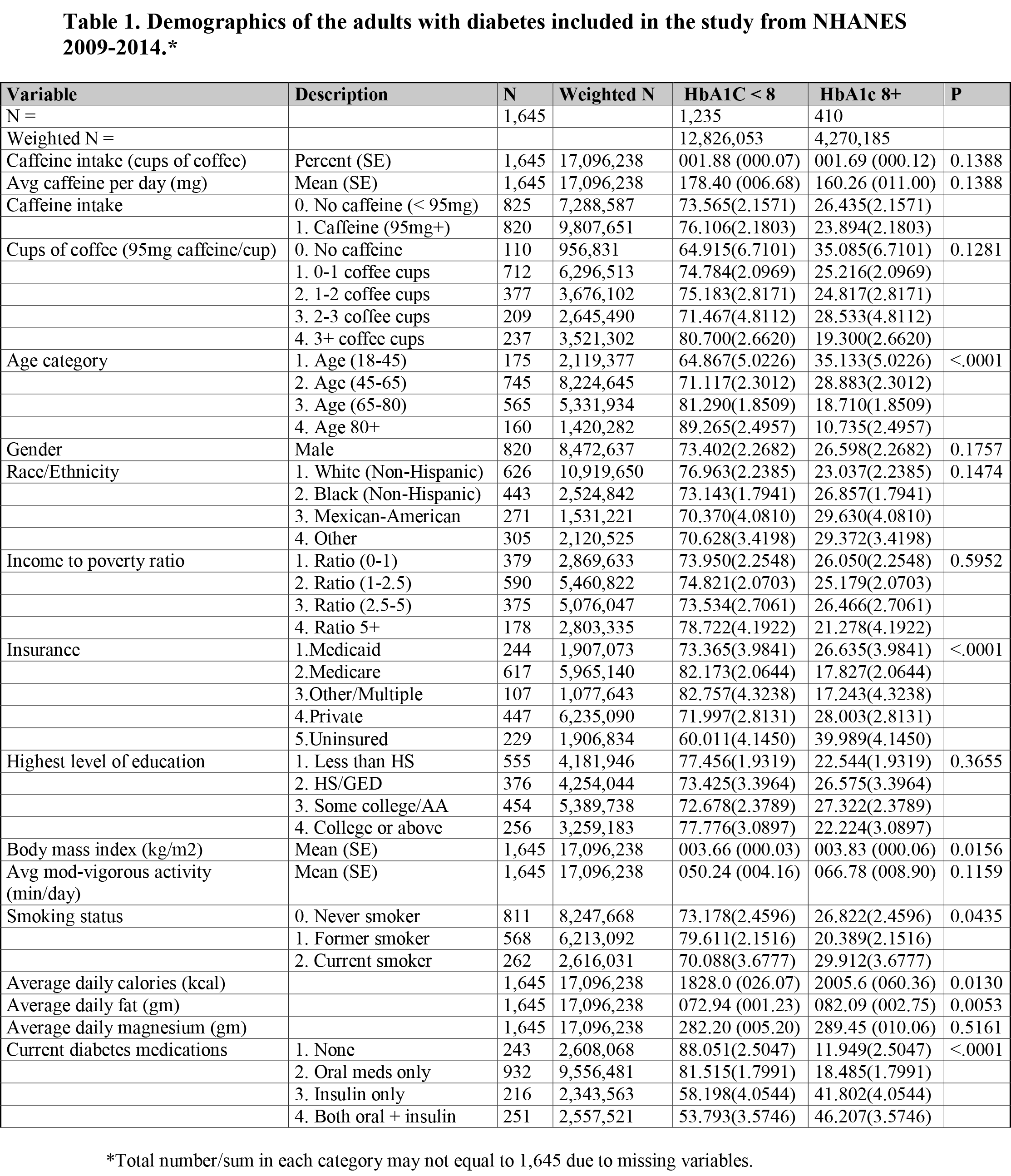
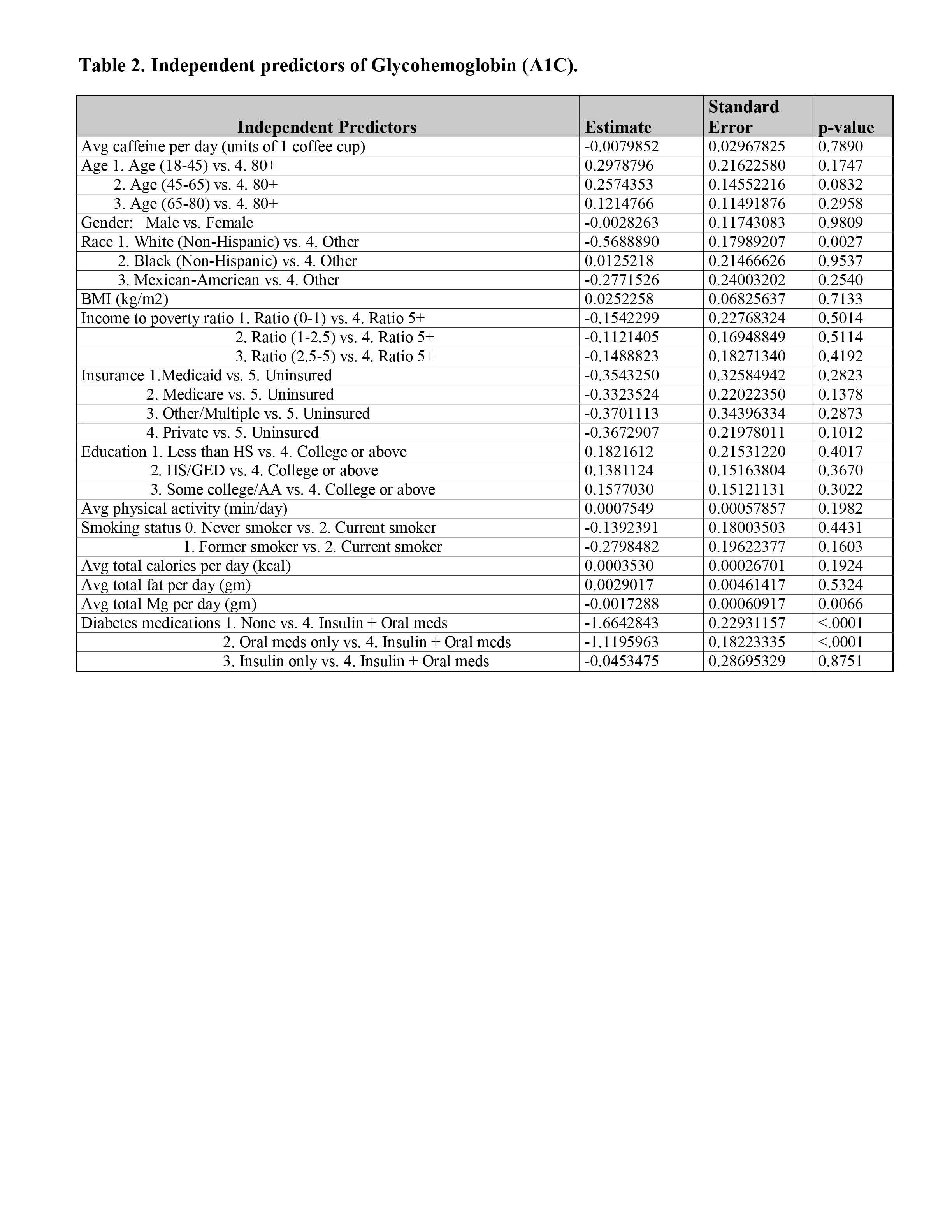
Results: There were total 1,645 adults with diabetes with complete caffeine intake and HbA1c representing a population of 17,096,238 (weighted for national estimate). The average caffeine intake was 1.83 (SE 0.06) cups of coffee. The average HbA1c was 7.31% (SE 0.05%). HbA1c (< 8 vs. 8+ percent) varied significantly with age, smoking status, calories and fat intake, and use of diabetes medications (Table 1). Caffeine intake (< 1 vs. 1+ coffee cups) varied significantly with age, gender, race, IPR, insurance status, education, smoking status, calories, fat, and magnesium intake. Caffeine was not a significant predictor of HbA1c in both univariate and multivariable linear regression analyses. The estimated change in HbA1c was -0.008 (SE 0.03) percent for every increasing 1 cup of coffee (p = 0.79) after adjusting for all other variables (Table 2).
Conclusions: Despite the established evidence on the protective effect of coffee consumption on the future development of diabetes, our study based on NHANES shows that it has no protective effect on people who already have diabetes. It is possible that coffee loses its protective effect once diabetes ensues. More longitudinal studies are needed to validate these findings.
Reference:
1) Van Dam RM, Hu FB. Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA 2005;294:97-104