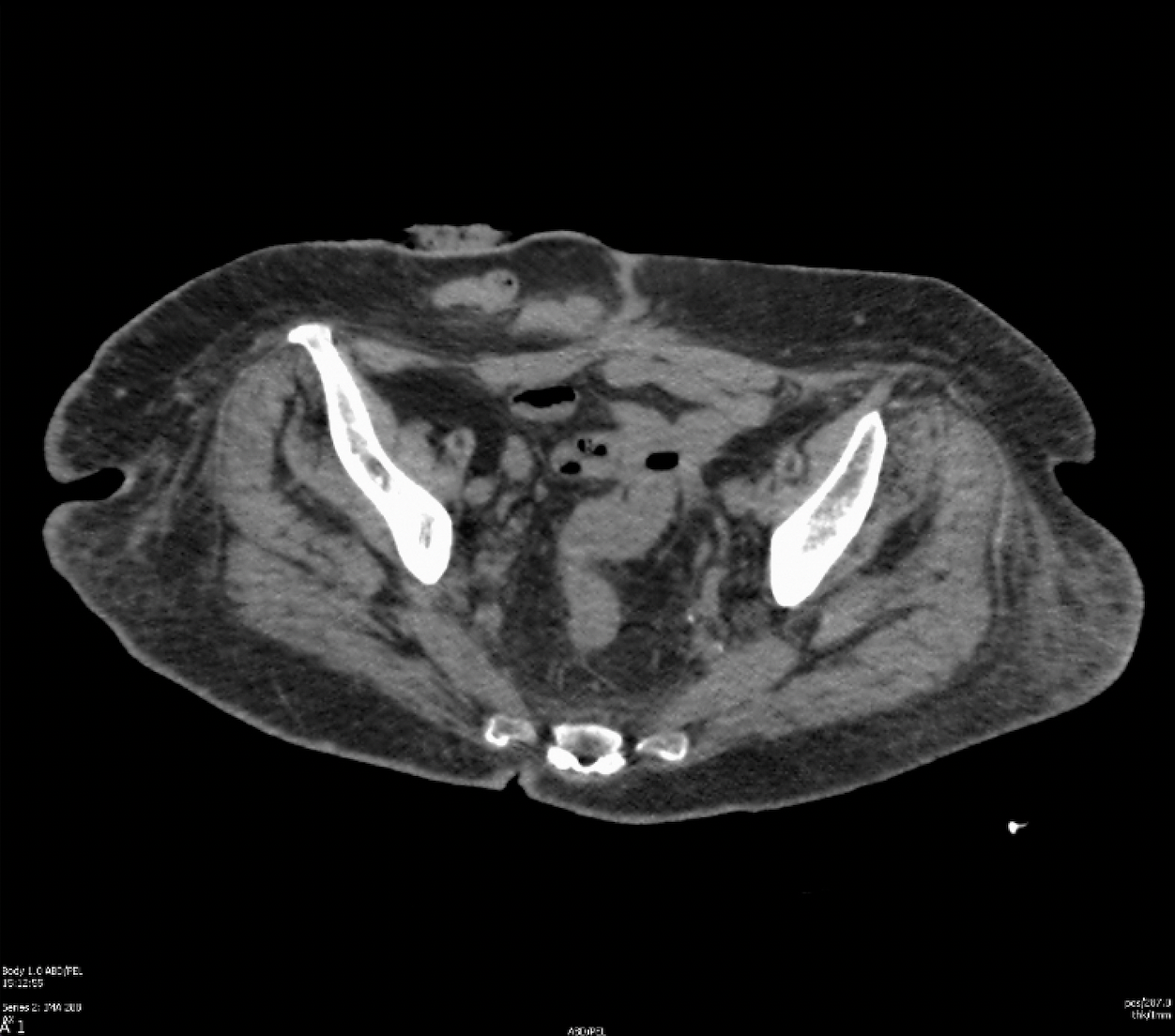
Case Presentation: A 71-year-old woman with a history of cecal perforation status post end ileostomy and subtotal colectomy in 2017 presented with intractable pain in the setting of a worsening erythematous intertriginous rash of the abdomen and labia. She reported using topical anti-fungal therapy without improvement of symptoms.Upon presentation, her vital signs were normal and laboratory findings were significant for a hemoglobin of 9.2 gm/dL and an albumin of 2.9 gm/dL. Computed tomography (CT) imaging revealed the sigmoid colon tethered to the vaginal cuff with intracavitary air favored to represent a colovaginal fistula. Dermatology was consulted and performed a punch biopsy of the abdomen which resulted as diffuse mixed inflammation with noncaseating granulomas with fibrosis, edema, and plasma cells consistent with cutaneous Crohn’s disease. CT enterography was performed with no evidence of active or chronic IBD. A colonoscopy demonstrated erythema and erosions in the remnant rectum with rectal biopsies demonstrating chronic colitis with patchy activity thought to be a sequela of her prior surgery. Ileal biopsies were normal. She was started on metronidazole and infliximab therapy for cutaneous Metastatic Crohn’s Disease (MCD) and discharged with outpatient follow up.
Discussion: The most common site for extraintestinal disease in patients with CD is the skin (2). Cutaneous MCD is a rare form of disease defined as noncaseating granulomas on histopathology from a skin lesion that is not contiguous with the GI tract or fistula (1,2). Interestingly, cutaneous MCD can occur before intestinal manifestations of CD which occurred in our patient case (2,3). As seen in our patient, cutaneous MCD causes significant morbidity including intractable pain (3,4). Due to its rarity, there have been no randomized controlled studies to guide treatment of cutaneous MCD (2,3). Case reports and case series have suggested treatment success with tumor necrosis factor (TNF) -alpha inhibitors, azathioprine, systemic steroids, and metronidazole (3,4). For this reason, our patient was started on both infliximab, a TNF-alpha inhibitor, and metronidazole therapy.
Conclusions: Cutaneous MCD is a rare disease that causes significant morbidity and can occur in patients without intestinal CD. In patients presenting with intractable pain in the setting of an erythematous intertriginous rash, cutaneous MCD is an important diagnosis to consider. Prompt diagnosis of cutaneous MCD is a crucial step in initiating appropriate treatment and alleviating suffering.