Background: ST-segment elevation myocardial infarction (STEMI) is a cardiac emergency that requires timely reperfusion preferably with cardiac catheterization. The coronavirus disease-2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV2), has adversely impacted the delivery of healthcare to patients with STEMI. Several process changes were observed across the world during this period, including alternative cardiac reperfusion protocols, supply chain shortages, redirection of resources, and delays in patient presentation as well as intervention.
Methods: This retrospective study utilized the 2020 NIS dataset, which is based on hospitalizations from January 1, 2020, to December 31, 2020. All patients who were 18 years of age and older and were admitted to the hospital with STEMI and COVID-19 infection were included in this study. The primary outcome was in-hospital mortality. Chi-square test was used to compare categorical variables and linear regression was used for continuous variables. For primary outcome, univariate logistic regression was used to calculate unadjusted odds ratio for variables of interest and p values of < 0.2 on univariate logistic regression was used to build multivariate logistic regression model to adjust for potential confounders[8]. A multivariate linear regression model was used for continuous variables (LOS and total hospital charge). A two-tailed p-value of 0.05 was considered significant.
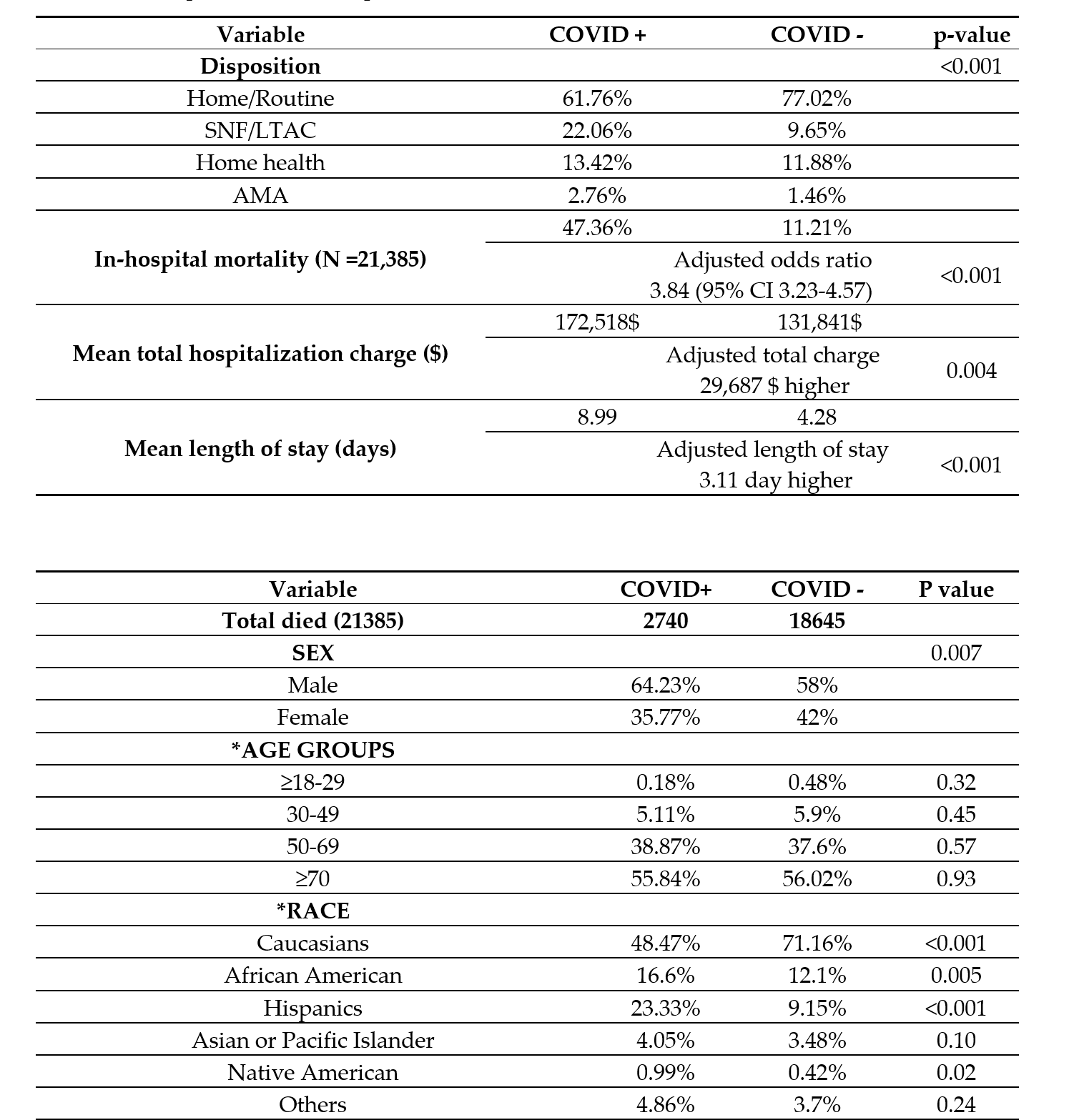
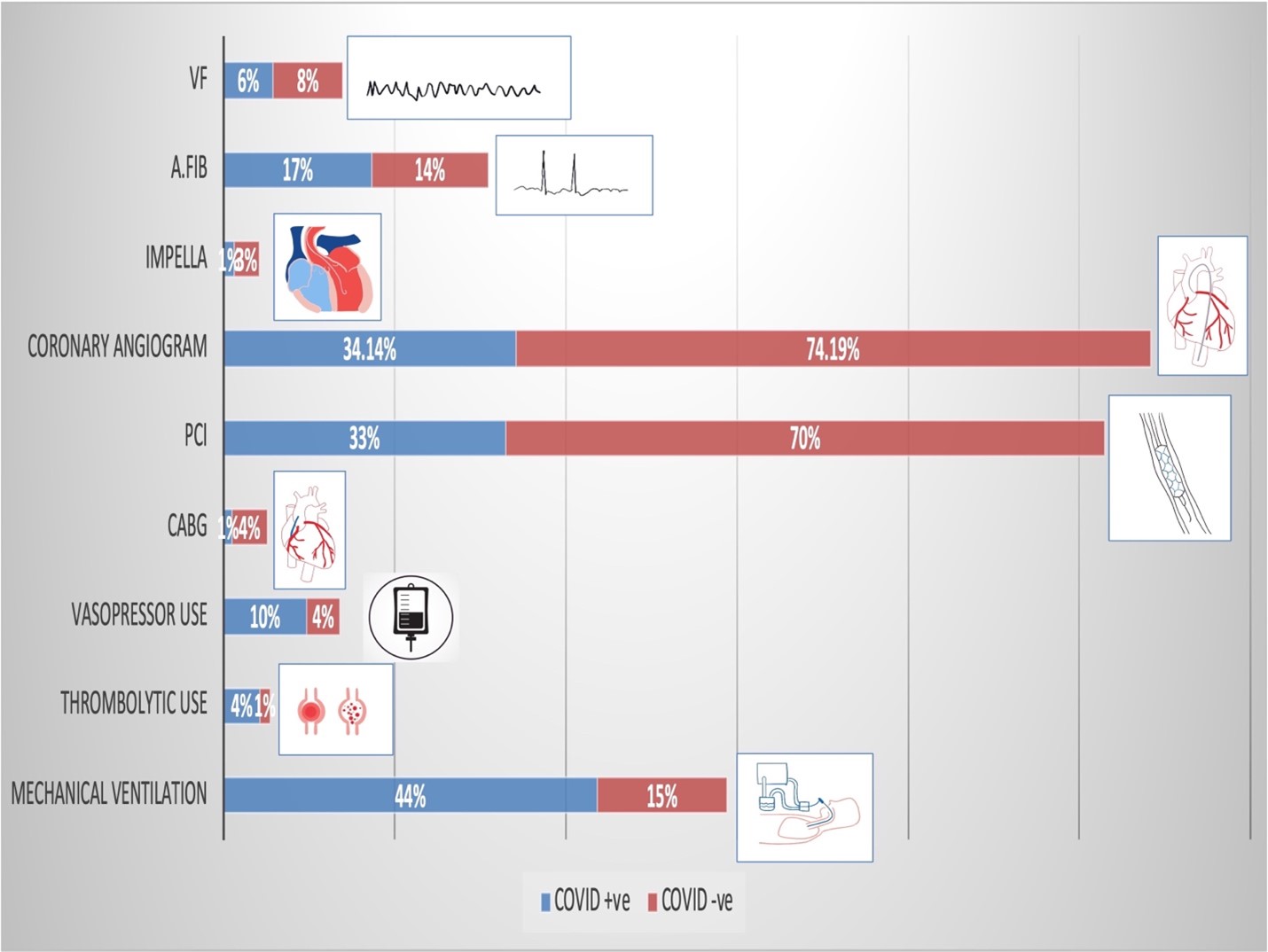
Results: Patients with STEMI and concomitant COVID-19 infection had a higher rate of inpatient mortality (47.4% vs. 11.2%, p < 0.001), increased length of stay (9 days vs. 4.3 days, p< 0.001) and higher cost of hospitalization (172,518 USD vs. 131,841 USD, p = 0.04) than those without COVID-19 in-fection. COVID-19 patients also received less invasive cardiac procedures (coronary angiograms: 30.4% vs 50.8%; P < .001, PCI: 32.9% vs. 70.1%, p< 0.001, CABG: 0.9% vs. 4.1%, p< 0.001) and were more likely to receive systemic thrombolytic therapy (4.2% vs. 1.1%, p< 0.001).
Conclusions: We conclude that STEMI patients with concomitant COVID-19 infection were nearly four times as likely to die in the hospital in comparison to non-COVID-19 patients. This finding is likely driven by both clinical complications of COVID-19 infection as well as system-wide alterations in delivery of cardi-ac care due to the healthcare burden of the COVID-19 pandemic. Thus, in addition to focusing on risk mitigation strategies for preventing infection during future pandemics, it is equally important to develop strategies for maintaining other critical clinical processes to allow for the delivery of healthcare to patients with life-threatening conditions such as STEMI in order to reduce unnecessary mortality.