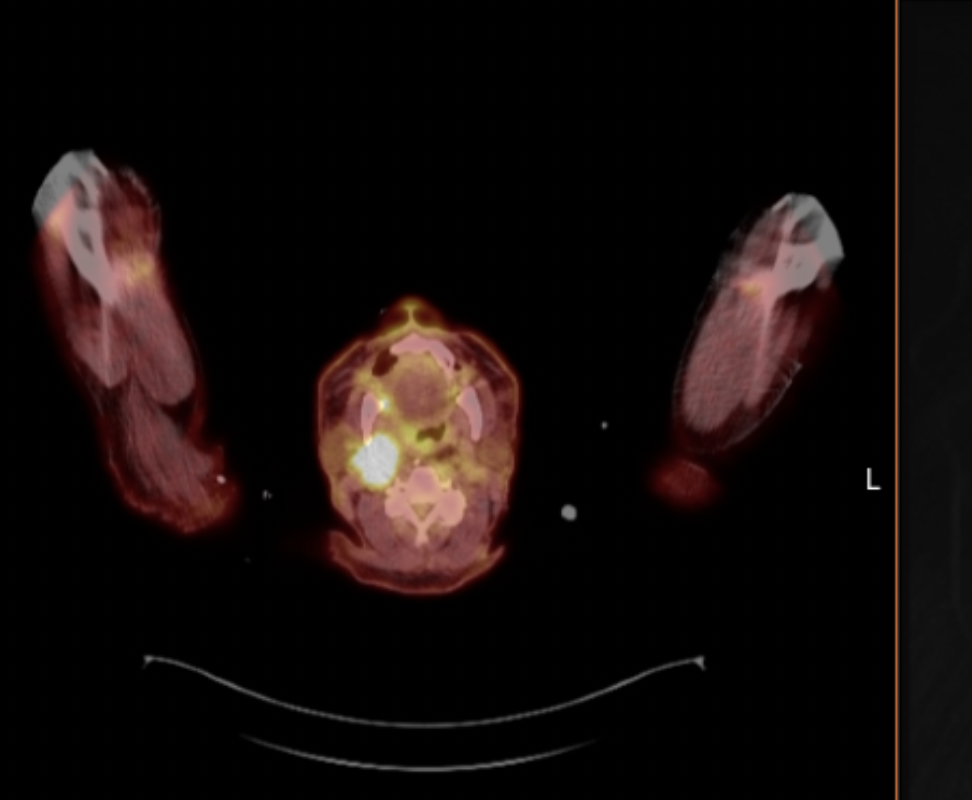
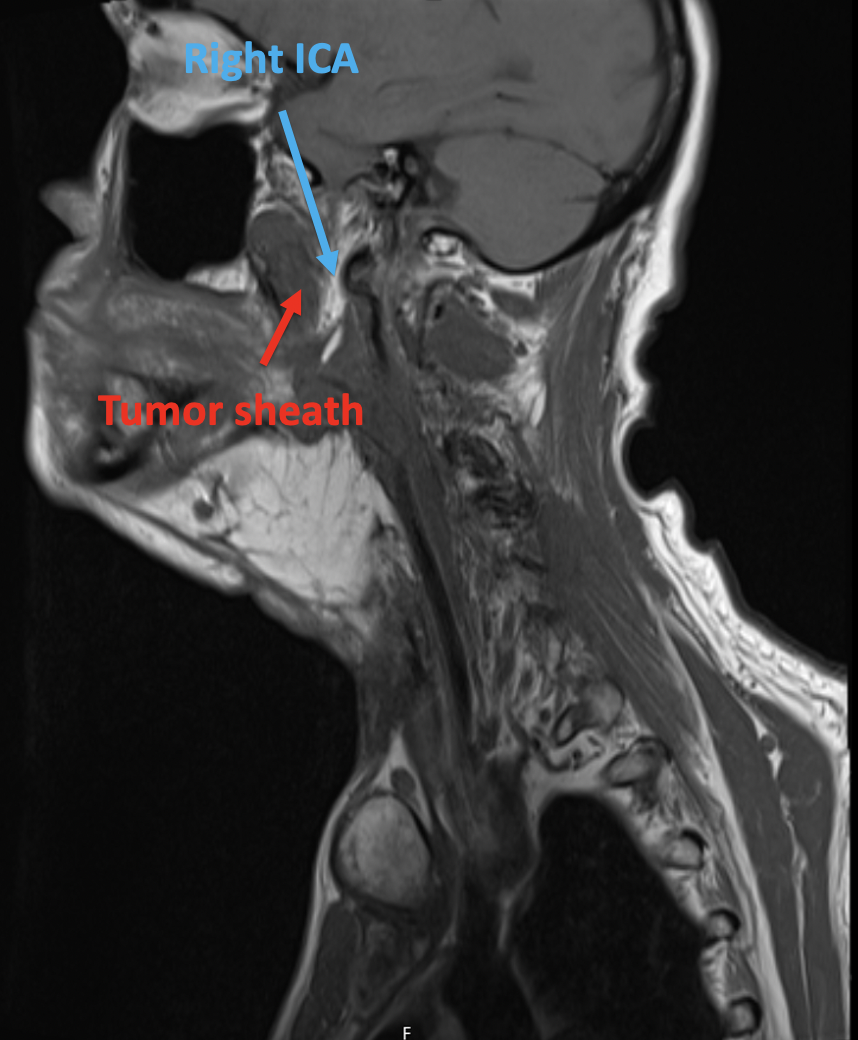
Case Presentation: 79-year-old man presented with recurrent syncope. He had a history of tonsillar squamous cell carcinoma (SCC) in 2005 s/p resection, pyriform sinus SCC in 2019 s/p total laryngopharyngectomy with tracheostomy and PEG placement. He had multiple prior admissions for the same presentation, which had been attributed to vasovagal syncope and dehydration from intermittent tube feed adherence. He had been started on midodrine 10mg TID. In the ED, orthostatic VS were positive; he received 3L of fluids with persistent symptoms. Admission ROS was otherwise notable for R sided jaw and neck pain out of proportion to exam. He was given several more liters of IV fluids but had repeated episodes of syncope. CT head/neck revealed abnormal soft tissue swelling along flap reconstruction. An FDG avid tongue base lesion in the right parapharyngeal region concerning for tumor recurrence was seen on PET CT, with a subsequent MRI neck demonstrating transfacial LN conglomerate involving the carotid sheath, including the R ICA and carotid bulb. He was diagnosed with carotid sinus syndrome with recurrent syncope secondary to malignant compression of the carotid sinus. He underwent an accelerated XRT course (24 Gy fractions in 3 fractions given 1x/weekly) due to poor tolerability of XRT sessions (he had recurrent presyncope) with significant improvement in his clinical symptoms.
Discussion: Syncope has many causes, and often requires careful history taking to elucidate leading diagnoses which can help guide further work up. The initial history in our patient led to a presumptive diagnosis of volume depletion but, once that had been excluded, additional causes were explored. Our patient’s history of head and neck cancer with recent onset jaw pain raised the possibility of tumor recurrence with compression of the carotid bulb triggering a condition called carotid sinus syndrome.Carotid sinus syndrome (CSS) describes a reflex syncope or near syncope caused by carotid sinus hypersensitivity, or a greater than normal decrease in heart rate or blood pressure as a result of carotid artery baroreceptor stimulation. It is an uncommon cause of syncopal episodes (< 1%). Direct compression of the carotid bulb is a rare cause of CSS, although there are multiple case reports documenting CSS secondary to both benign and malignant neck masses. Palliative XRT has been described in this clinical scenario previously, as surgical resection is rarely feasible given carotid involvement. The particular regimen used in this case has been shown to have a high response rate of both symptomatic relief and tumor shrinkage (~80%).
Conclusions: CSS secondary to malignant compression of the carotid bulb is a rare cause of unexplained syncope. This case encourages providers to maintain a broad differential for patients who present with unexplained syncope without clear triggers, particularly in patients with recurrent episodes and in those with a history of head and neck cancer. Palliative XRT with or without chemotherapy is often the best management when malignant tumors are the cause.