Background: The use of point-of-care ultrasound (POCUS) by hospitalists is rapidly evolving and is variable between hospital medicine groups and individuals. Although POCUS has been shown to increase patient satisfaction in the emergency department and primary care settings, little is known about hospitalized patients’ perspectives on POCUS in their care. POCUS allows patients the opportunity to visualize and discuss diagnostic findings in real-time with their treating hospitalist, which may improve their understanding and satisfaction with their medical care. We sought to better understand patient satisfaction with POCUS in domains included in the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey as well as a previously validated survey instrument to assess patient satisfaction with POCUS.
Methods: We conducted a survey of 45 medical inpatients at a single U.S. academic medical center in the Mountain West region who underwent POCUS during their hospitalization. We included patients who had any POCUS exam performed by their attending hospitalist as part of usual medical care. We only considered patients of hospitalists who self-identified as regular POCUS users. The institutional review board approved our study. We excluded patients who were altered or did not speak English. Patients who consented to participate were administered a 10-question survey by a research team member not involved in their clinical care on the same day of their POCUS exam. Survey questions were adapted from validated survey instruments regarding satisfaction with POCUS or HCAHPS survey questions. Responses were collected on a 5-point Likert scale. For this analysis, “strongly agree” and “agree” were grouped, as were “strongly disagree” and “disagree.”
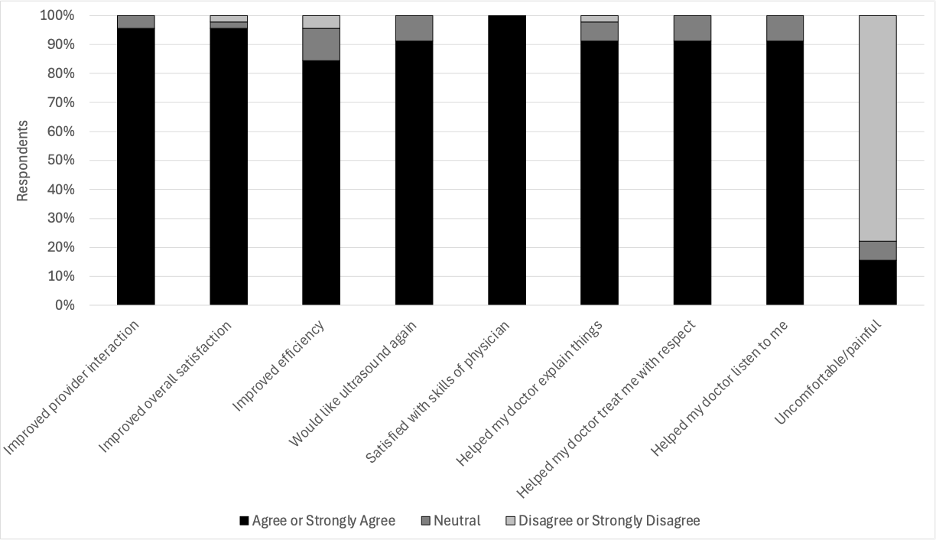
Results: We surveyed 45 medical inpatients regarding their satisfaction with POCUS performed by their attending hospitalist as part of their routine medical care. Respondents reported a high degree of satisfaction with the inclusion of POCUS in their care (Figure 1). 96% of respondents reported that POCUS improved their overall satisfaction with their care. Respondents also reported that POCUS improved their hospitalists’ ability to interact with them (96%), explain things (91%), treat them with respect (91%), and listen to them (91%). Although POCUS was well tolerated, 16% of respondents reported that it was uncomfortable or painful.
Conclusions: This study is among the first to assess patient satisfaction with hospitalists’ use of POCUS. Patients were highly satisfied with the inclusion of POCUS in their care across multiple domains surveyed. Notably, patients reported that POCUS positively impacted their perception of their hospitalist’s listening and communication skills, which are asked in the HCAHPS survey of patients. This may be due to POCUS promoting bedside interaction and real-time visualization, facilitating discussion of diagnostic findings and treatment options between patients and hospitalists. An important strength of our study is the inclusion of subjects who underwent POCUS as part of real-world hospitalist-performed POCUS at an academic medical center. Limitations of this survey include a relatively small sample size, the inability to stratify results by subgroups (such as different POCUS exams or indications), and the lack of a control group that did not undergo POCUS. Further work should investigate how patient satisfaction is impacted by efforts to support hospitalist use of POCUS.