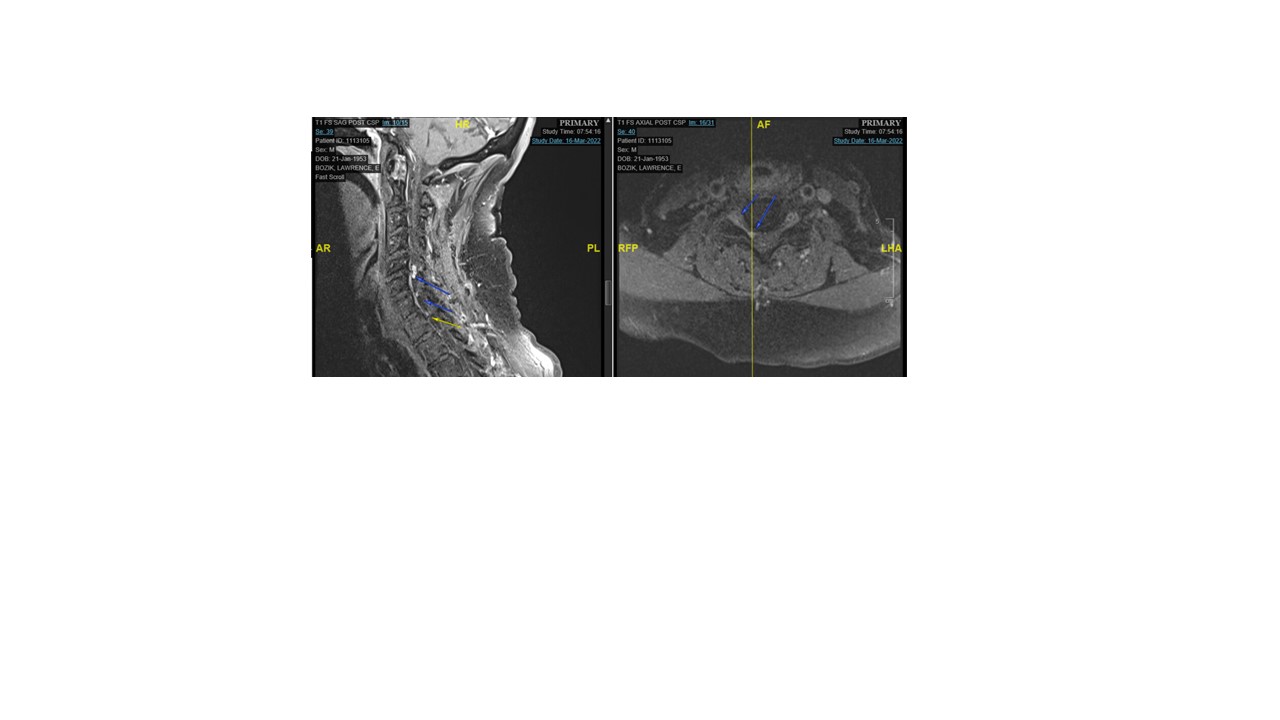
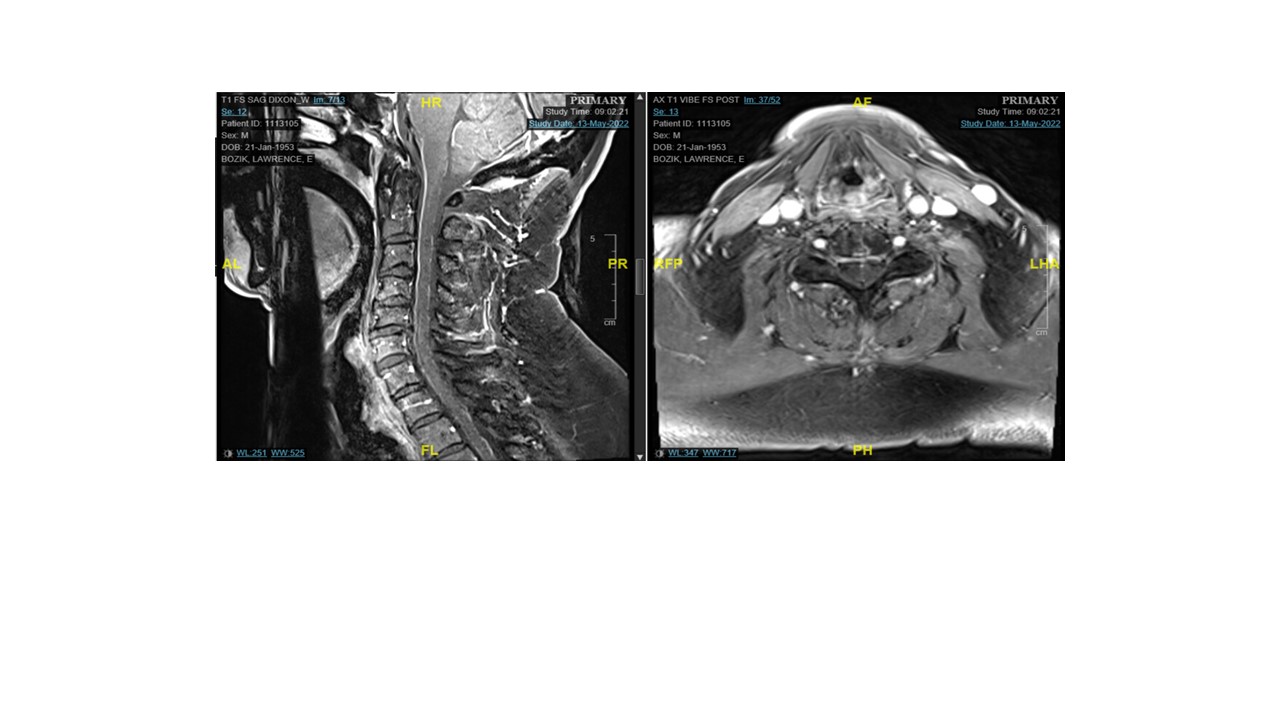
Case Presentation: A 69-year-old male with a past medical history of urothelial carcinoma status post left nephrectomy began immunotherapy and was started on Atezolizumab. He developed bilateral lower extremity weakness that began following his first dose. After 3 doses, in 02/2022, his lower extremity weakness worsened to the point where he could not walk. A Nerve Conduction Velocity (NCV) study was performed and was consistent with acute demyelinating polyneuropathy. A cervical MRI showed an enhancing lesion at C6-C8. He was treated with 3 days of intravenous methylprednisolone every 6 hours for 3 days followed by 5 days of .4gm/kg Intavenous Immunoglobin (IVIG). He regained his ability to walk after IVIG treatment. The enhancing lesion noted on MRI remained. 3 weeks after the first IVIG treatment, he declined significantly, redeveloping symptoms where he could not ambulate and required assistance to use the toilet. He had no lower extremity reflexes and loss proprioception of his hands. Lumbar puncture with albuminocytological dissociation with negative cytology. Serum antiganglioside antibody tests were negative. He was scheduled for another IVIG infusion at .4gm/kg followed by a dose of IVIG .6gm/kg the next day, and then 4 more days of IVIG .25gm/kg. His lower extremity weakness and difficulty walking remained the same so he was arranged for plasmapheresis x 5 cycles. His weakness improved substantially, reflexes returned, and he no longer had proprioceptive loss of his hands. A cervical MRI obtained 1 month after plasma exchanged (PLEX) showed resolution of the C6-C8 enhancing lesion. He is now ambulating with a cane. This case highlights the effectiveness of plasma exchange in a case that was refractory to IVIG.
Discussion: The use of immune checkpoint inhibitors (iCPI) in the treatment of cancer has gained prominence due to their effectiveness. Unfortunately, neurological immune-related adverse events (irAEs) represent a growing problem in hospital medicine. Many of these cases are rare but may have serious consequences when they occur. One reported iRAEs is Acute Inflammatory Demyelinating Polyneuropathy (AIDP) also known as Guillan-Barre Syndrome (GBS). To our knowledge there is one reported case of Atezolizumab induced AIDP in the literature. Here we report a case of a 69-year-old male with urothelial carcinoma s/p left nephrectomy who developed Atezolizumab induced AIDP that was refractory to IVIG requiring treatment with plasma exchange (PLEX).
Conclusions: To our knowledge, this is the first reported case of Atezolizumab induced AIDP that is refractory to IVIG but responded to Plasma Exchange (PLEX). PLEX can be effective as treatment for Atezolizumab induced AIDP that is refractory to IVIG. When to initiate PLEX for immune checkpoint inhibitor induced AIDP is unclear and warrants further investigation.