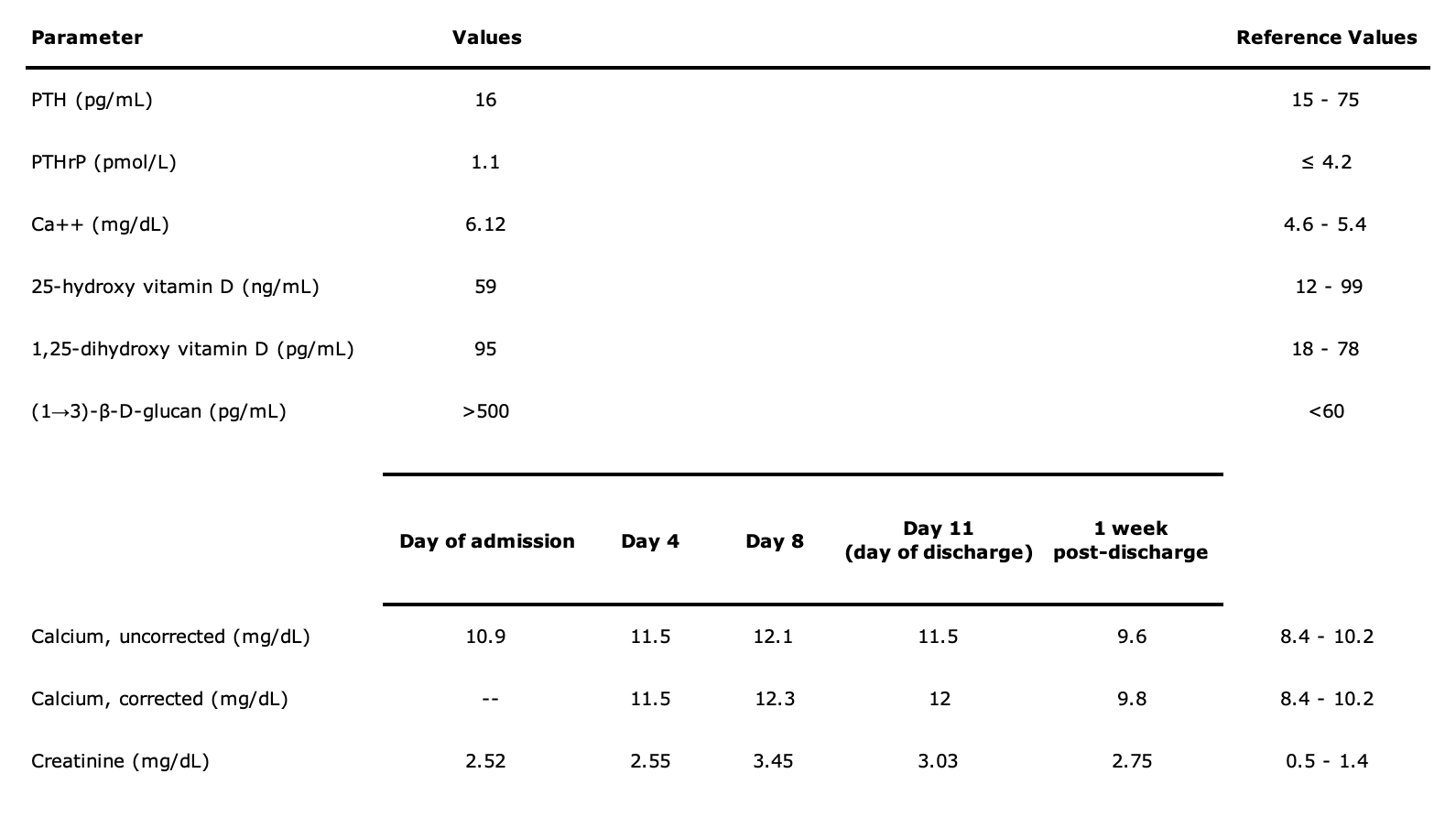
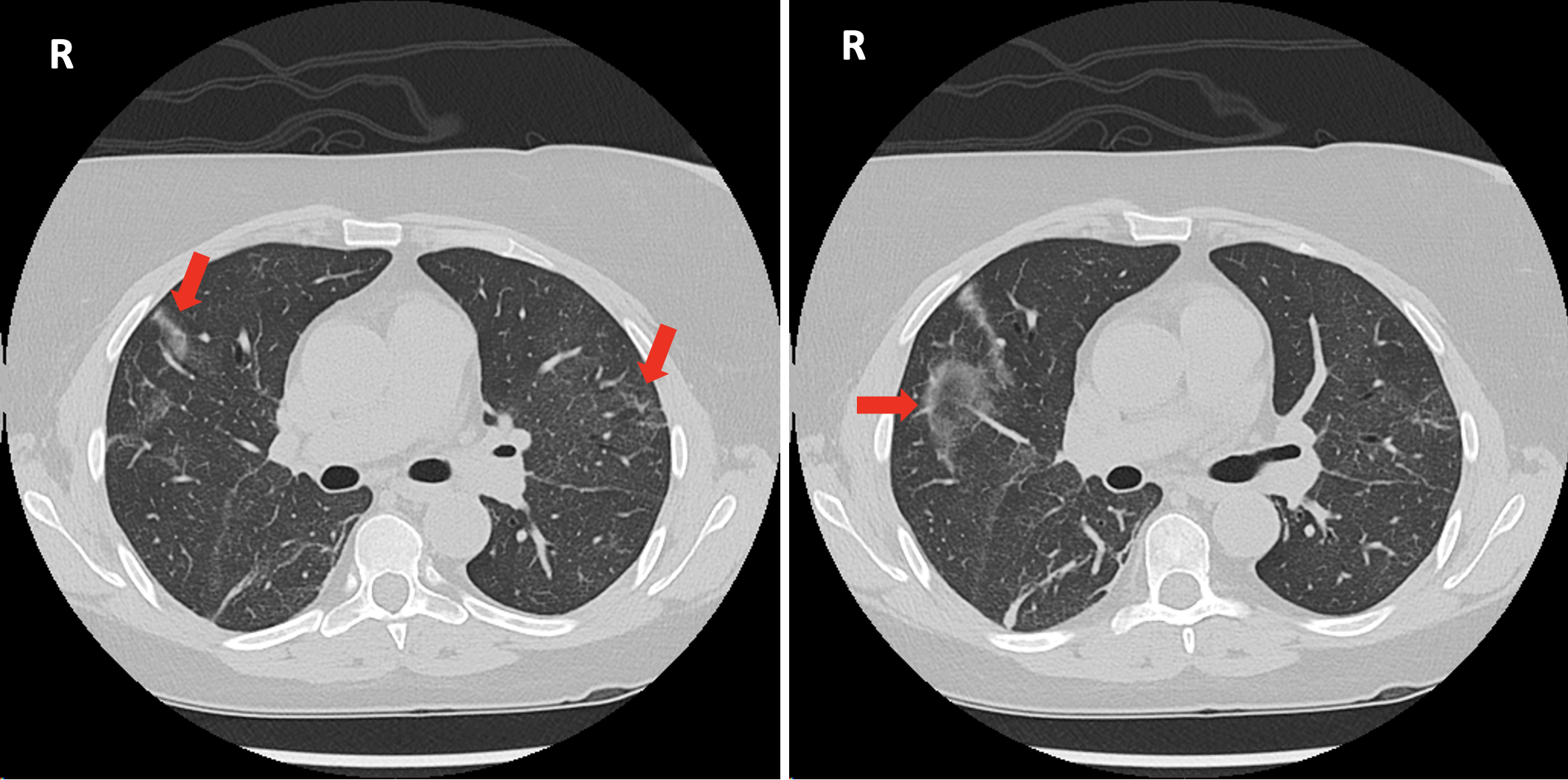
Case Presentation: A 55-year-old woman with a remote history of renal transplant complicated by stage 4 chronic kidney disease (CKD) presented to the emergency room with a week history of progressive fatigue, fever, dry cough and exertional dyspnea. Outpatient medications were tacrolimus 2.5mg BID, mycophenolate mofetil 500mg BID, prednisone 5mg daily, and vitamin D 1000 units daily.Vitals on presentation were temperature of 100.6 degree F, respiratory rate of 18-22 per minute, blood pressure of 130-170/90-110 mmHg, heart rate of 80-100 beats per minute and normal oxygen saturations. Physical exam was non-significant except for mild use of accessory muscles of respiration. Pertinent laboratory parameters on admission and during hospital stay are shown in Table 1. Infectious work up of blood & respiratory cultures, urine Pneumococcal & Legionella antigens, and chest X-ray were unrevealing. A CT scan of chest showed scattered ground glass lung opacities (Figure 1). Infectious disease team deferred antibiotics given overall stability pending work up and recommended bronchoscopy.On day 4, she had respiratory decline with hypoxemia needing supplemental oxygen. Labs concomitantly showed increasing corrected calcium level of 11.5 mg/dL peaking to 12.3 mg/dL and rise in creatinine to 3.11- 3.45 mg/dL. Intravenous fluids were started. Vitamin D was discontinued. Bronchoscopy and lavage was performed. Given findings, empiric treatment for Pneumocystis jirovecii pneumonia (PJP) was started with trimethoprim/sulfamethoxazole and high dose steroid. Hypercalcemia work up revealed elevated 1,25-dihydroxy vitamin D to 95 pg/mL. Fungitell assay was elevated with (1,3)-beta-D-glucan levels >500 pg/mL. Her condition rapidly started improving with treatment for PJP and she was discharged with 1 week follow up. The patient was doing well on follow-up and repeat labs showed corrected calcium level of 9.8 mg/dL with creatinine back to baseline.
Discussion: PJP is an opportunistic infection impacting immunocompromised hosts. In renal transplant patients, the incidence is 5-15% with mortality rates ranging 13-38%. Respiratory symptoms are the predominant feature, but occasionally unusual presentations can occur. Non-parathyroid mediated hypercalcemia has rarely been associated with PJP in general, but it has relatively higher prevalence in kidney transplant patients when compared to other immunocompromised hosts. Exact mechanisms explaining predisposition of renal transplant recipients to PJP associated hypercalcemia remain unclear, but in the setting of relatively suppressed PTH and elevated 1,25 dihydroxy vitamin D, as in our case, an increased production of 1-alpha hydroxylase by pulmonary alveolar macrophages from PJP granulomatous lung involvement remains the leading hypothesis.Vitamin D supplementation is common in renal transplant patients with CKD and can provide an increased substrate (calcidiol) for 1-alpha hydroxylase with resultant hypercalcemia. In addition to the usual management of hypercalcemia, discontinuing calcium/vitamin D supplements & initiating treatment specific for PJP is important due to suggested inhibitory effects of steroids on extrarenal 1-alpha hydroxylase enzyme.
Conclusions: PJP infection can result in hypercalcemia in renal transplant recipients especially while on vitamin D supplementation. Medical providers should keep a high index of suspicion for PJP when hypercalcemia is noted in this patient subgroup even with non-classical presentation.