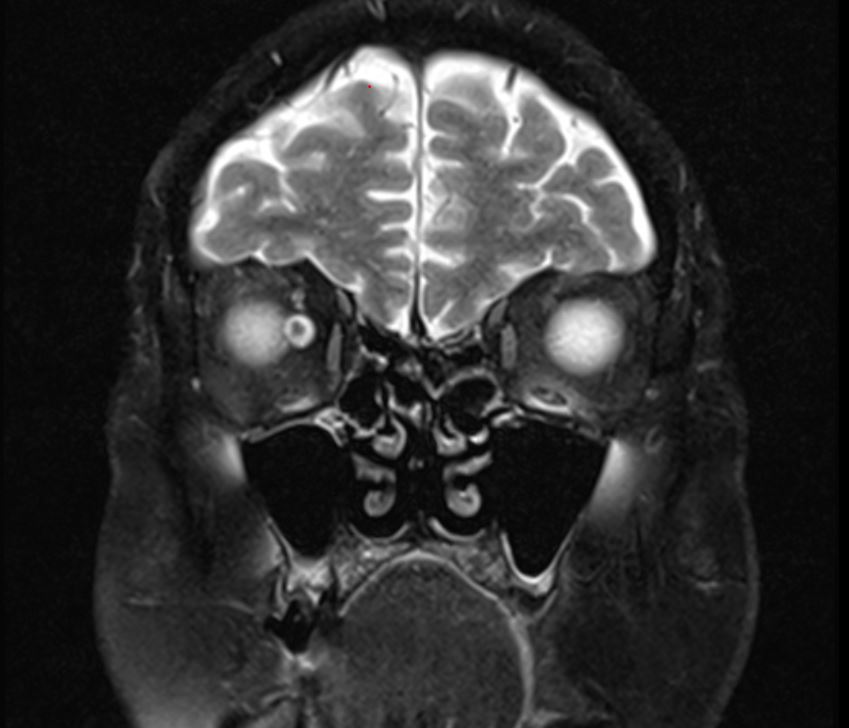
Case Presentation: 80-year-old retired bus driver was admitted to the ER after multiple falls at home, generalized weakness, back pain and body aches. Patient developed generalized weakness over the last two weeks. Patient reported four-day history of blurry vision involving the right eye and observed drooping of the right eyelid over the past two days almost to shut eye with no pain. He denied headache, difficulty in swallowing, weakness of the limbs, or bladder or bowel incontinence. He as well denied fevers, chills, cough, sputum, or diarrhea. His past medical history significant for multiple myeloma diagnosed two years ago in remission, chronic urinary retention, hypertension, hyperlipidemia, diabetes, glaucoma, compression fractures requiring braces at home, osteoporosis and malignant melanoma at the back. Initial examination did not show any facial asymmetry, and palate was symmetric and uvula in the midline. Tongue was in the midline. The patient was alert, awake and oriented and had no aphasia or dysarthria, intact motor power of all extremity with no arm or leg drift. Initial suspicion was for an isolated third nerve neuropathy, likely from diabetes.Patient had imaging studies done including, CT Angiogram of head, MRI Brain, MRI C Spine and MRI Orbits. MRI orbits showed abnormal enhancements in the cisternal segments of each cranial nerves 3,5 7 and 8. The appearance of the globes and extraocular muscles were normal. Finally lumbar puncture done, with cloudy yellow CSF drained and sent for laboratory examination. CSF examination was highly abnormal with protein elevated at 600 giving yellow tinge. There were large number of abnormally large plasmacytoid cells. All of these pointed towards a carcinomatous meningitis with diffuse involvement of the neuraxis.
Discussion: The monoclonality of the cells identified in the CSF matches that of the initial diagnosis of the myeloma in our patient. Stand-alone case reports and case series exist, where ocular symptoms like diplopia was the only manifestations of multiple myeloma. A systematic approach to rule out central and peripheral causes of diplopia may be helpful. Peripheral myositis of the extraocular muscles, injury to the globe, superior orbital fissure syndrome, involvement of the cranial nerves in the cavernous sinus, vascular lesions of the brain and neuroinflammatory lesions like GBS may all be contributory to the development of diplopia. In our patient the CSF examination could help us arrive at diagnosis quickly. CSF remains the gold standard of diagnosis. It is also appreciated that a multi-disciplinary team approach with independent evaluations of the neuroradiologic findings is contributory to patient diagnosis and management. Arrival at a quick diagnosis is important to offer treatments like whole brain radiotherapy immediately. Prognosis remain highly guarded in these circumstances of extensive spread of the multiple myeloma to the central nervous system.
Conclusions: The presentation of our patient highlights few important aspects in clinical care of subjects affected with multiple myeloma. The CSF examination helped us arrive at diagnosis. A high degree of suspicion is needed to arrive at a diagnosis of leptomeningeal myelomatosis which is very rare and has high mortality rate. Clinical outcomes in these patients always run a rapid downhill course.