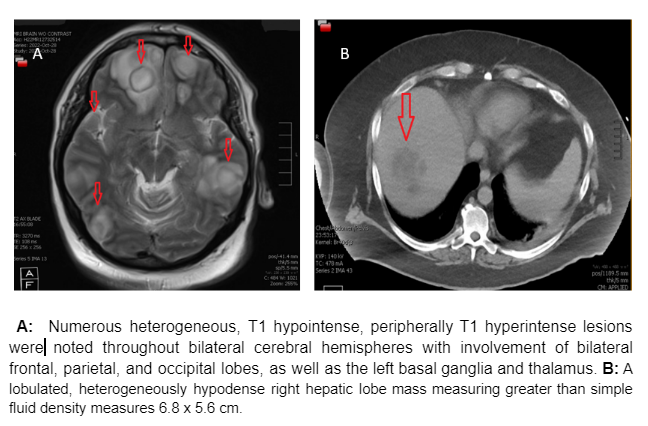
Case Presentation: We present a case of a 44-year-old male with a history of FN liver abscess, diagnosed two years ago (treated with four weeks of ertapenem to complete resolution), who was brought to the emergency department with confusion, expressive aphasia, fever, and ataxia for three weeks. The patient was vitally stable. Lab workup showed leukocytosis. A CT brain revealing numerous hypodense lesions in the brain was followed by an MRI, which was significant for ring-enhancing lesions. A CT abdomen/pelvis showed a 6.8 cm lobulated mass in the liver and focal thickening of the sigmoid colon concerning malignancy. Broad-spectrum antibiotic coverage with Ceftriaxone, Vancomycin, and Flagyl was initiated. CSF analysis showed mild elevation of protein 143 mg/dl (15-45 mg/dl) and normal white blood cell counts and glucose. Additional fungal, bacterial and protozoal workup was unremarkable. Hepatic abscess drainage was purulent without any staining or growth on culture. On day six plan was made to do a diagnostic biopsy/drainage of intracerebral lesions.Further molecular testing was obtained, including Karius testing and Nextgen sequencing. Anaerobic and aerobic blood culture bottles were drawn on admission and showed no growth for one week. Fusobacterium nucleatum was identified in brain biopsy culture using 16/18S rRNA sequencing on day ten. The patient improved clinically over the next few days, and all studies returned negative. A prolonged antibiotic course of ceftriaxone and metronidazole was planned to cover for possible resistant organisms since no other new source of infection was identified. Also, colonoscopy and repeat brain imaging in six weeks was proposed.
Discussion: FN is a gram-negative anaerobic bacteria. As FN are part of the normal microbiota of the oral cavity, there is a strong association of FN with periodontal diseases [1,2]. Though not entirely well understood, FN also plays a role in various extraoral disease processes, such as colorectal cancer, chorioamnionitis, Lemierre’s syndrome, and abscess formation [3]. Cases of simultaneous liver and brain abscess formation due to FN are rare but have been reported [4]. Nonetheless, our report describes the finding of a new-onset brain abscess and recurrent liver abscess from FN infection in an immunocompetent patient [4].Literature review shows that culture is the predominant method for diagnosing FN infection in most cases. It is also studied blood cultures may have poor sensitivity for FN diagnosis, especially in association with abscesses. However, PCR is performed infrequently. Still, PCR-mediated amplification and sequencing of 16S ribosomal RNA appear useful if an anaerobic pathogen is likely, but conditions are not optimal for recovery. 18S PCR is the highest yield in patients at risk of fungal disease [5].
Conclusions: The use of new diagnostic modalities, including 16S and 18S rRNA Gene PCR, has become the standard practice for diagnosing culture-negative brain abscesses. Diagnosing fusobacterium nucleatum (FN) abscesses in clinical settings, however, continues to remain a challenge.