Background:
The Agency for Healthcare Research and Quality (AHRQ) has adopted iatrogenic pneumothorax (IAP) as a zpatient safety indicator. From 2006 to 2007 our institution was ranked within the lowest United Healthcare Consortium performance quartile for IAP. In response, we established a multidisciplinary team to reduce our rate of IAP.
Purpose:
A quality improvement (Ql) Team was formed with representatives from the departments of medicine, surgery, critical care, anesthesia, emergency medicine, simulation, nursing, and hospital quality. We performed a detailed analysis of all 2006‐2007 IAP and identified 3 important findings: (1) the majority of lAPs were due to central venous catheter (CVC) placement, of which 70% were from the subclavian approach; (2) some IAP occurred with inadequately supervised house staff; and (3) medical record documentation of CVC placement was poor. Our goal was to reduce the rate of IAP from CVC placement by 50%. Our strategy used evidence‐based medicine to promote ultrasound guided IJ as method of choice for CVC placement.
Description:
Implementation was carried out in 2 phases. In phase 1 (physician education), we developed a Web site curriculum for IJ ultrasound‐guided CVC placement. In addition, a CVC simulation program was created for ultrasound guided IJ placement in our simulation center for all incoming medical, surgical, anesthesia, and emergency medicine interns. To reinforce the curriculum's teaching and to disseminate this information more widely, we created 2 educational tools: (1) a checklist with evidence‐based practices for CVC placement distributed via central line kits and educational flyers, and (2) CVC procedure note template with California Department of Public Health documentation requirements. In phase 2 (culture change/physician buy‐in), leaders of our critical care and surgical services promoted ultrasound guided IJ as the method of choice for CVC placement. The subclavian approach was limited to cases in which the ultrasound guided IJ was contraindicated or not available. Our institutional policy requires that the first 5 CVCs by residents be supervised by a physician who has successfully inserted and documented the placement of 5 CVCs. In our ICU, all CVC placement by residents is supervised by an ICU fellow or attending.
Conclusions:
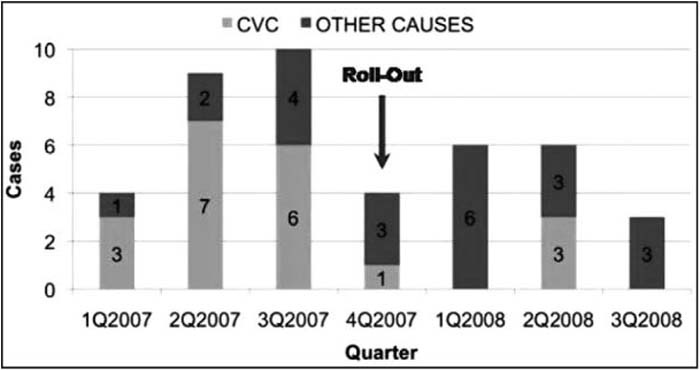
After implementation of the processes described, CVC‐related IAP cases decreased from 16 (1Q07‐3Q07) to 4 (4Q07‐3Q08), more than a 75% reduction in CVC‐related IAP. Through a multidisciplinary Ql effort, we significantly reduced the number of CVC‐related lAPs. Acombination of strong leadership, evidence‐based practice tools, standardization, supervision, and simulation training enabled the necessary culture change to improve the safety of placing CVCs.
Author Disclosure:
L. Shieh, none; P. Maggio, none; F. Mihm, none; J. Lee, none; D. Sedehi, none; K. Bowes, none; L. Meinke, none; I. Tokareva, none; N. Szaflarski, none; J. Hopkins, none.