Background:
Research into post discharge risk has emphasized medical comorbidity with less consideration of patient functional status and social support. The Patient‐Reported Outcome Measurement Information System (PROMIS) is an inventory of NIH‐funded, publicly available measurements of function. Using PROMIS instruments we surveyed elders at hospital discharge and afterward to characterize physical, cognitive, social and emotional functional status and its relation to post‐discharge utilization.
Methods:
We prospectively surveyed patients ≥65 years of age being discharged home. Participants completed computer adaptive testing modules of physical function, applied cognition, emotional distress (depression and anxiety), ability to access social support, and affective experience of social isolation. Participants were contacted by phone at 3 and 30 days after discharge for reassessment. We abstracted sex, race, age, Charlson Score, ED utilization in the 6 months prior to admission, acuity of admission and index length of stay (LOS) from the medical record. We performed difference testing to examine function in the study population compared to an age‐matched cohort. We conducted multiple logistic regression to determine the relationship between functional status and rehospitalization.
Results:
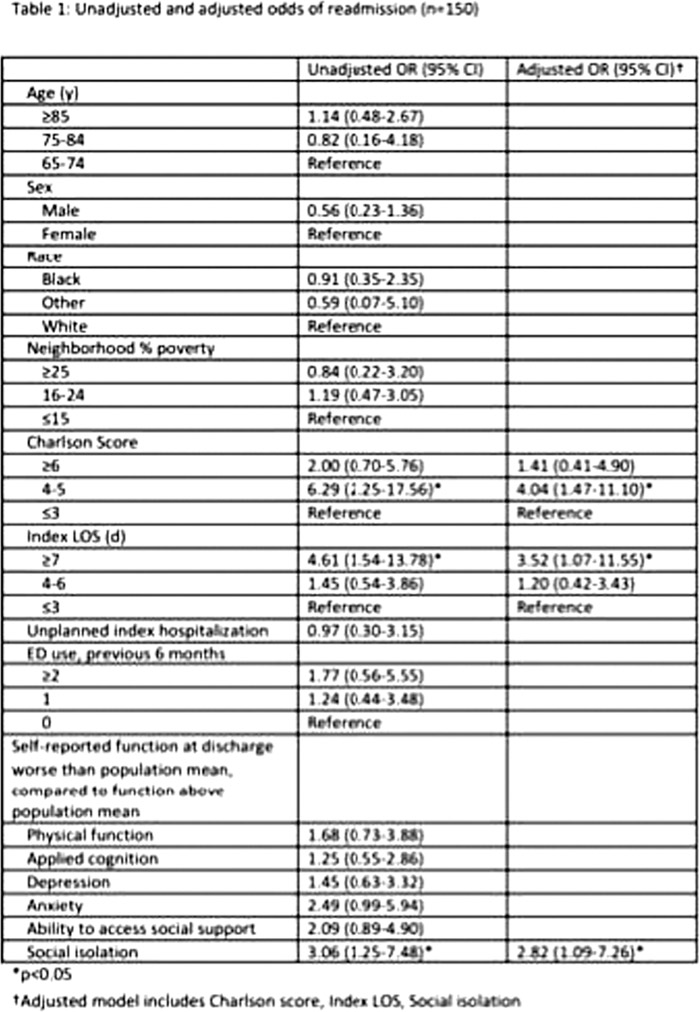
Baseline data were obtained on 237 patients, 150 of whom were contacted at 30 days after discharge (63.3%). Bivariate testing showed significant associations between 30‐day readmission and LOS, Charlson score and social isolation. There were no significant associations observed between readmission and 6 month ED utilization, anxiety, depression, physical function, ability to access social support, cognitive function, neighborhood poverty concentration, sex, age or race.(Table 1) In multiple regression analysis including the above significant variables, individuals in the study cohort with a social isolation score above the mean experienced 2.82 (95%CI 1.09‐7.26) higher odds of rehospitalization compared with individuals reporting below average isolation. A model including the above significant variables as well as acuity of admission and 6 month ED utilization was associated with a c‐statistic of 0.78.
Conclusions:
The self‐reported measure of social isolation included in PROMIS is independently associated with rehospitalization risk. Measurement of social isolation in assessment of readmission risk may improve intervention effectiveness as well as risk standardization for purposes of readmission performance‐based incentives.