Background: Bronchiolitis is one of the most common reasons for hospitalizations in children with > 100,000 admissions each year. High-flow nasal cannula (HFNC) therapy has been widely adopted to treat bronchiolitis with increasing use outside of the pediatric intensive care unit (PICU). The use of oral feeding while on HFNC has been questioned due to concerns for safety, perceived swallowing dysfunction, and risk of aspiration, resulting in high variability in practice. Our objective was to determine the incidence of adverse feeding events and aspiration pneumonia among children admitted with bronchiolitis and allowed to receive oral nutrition while on HFNC.
Methods: We conducted a single-center, retrospective chart review in a large tertiary children’s hospital from March 2017 to May 2020. We included children 2 months to 2 years of age admitted for bronchiolitis and treated with HFNC (2L/kg up to a maximum of 12L) on the pediatric ward. We excluded patients with chronic medical conditions, chronic lung disease, congenital heart disease, bacterial pneumonia, and those placed initially on nasal CPAP (nCPAP). Primary outcomes included incidence of adverse feeding events and aspiration pneumonia, defined as clinical or radiographic evidence of aspiration pneumonia or pneumonitis. Secondary outcomes included escalation of respiratory support to nCPAP, PICU transfer, NPO status, length of time NPO, length of stay (LOS), 7-day readmission, use of IV fluids, and feeding characteristics. Frequencies, means (standard deviation), or medians (IQR) were used to describe the sample. T-tests or Mann-Whitney tests were used to compare sample characteristics between those who were made NPO vs. not during the admission.
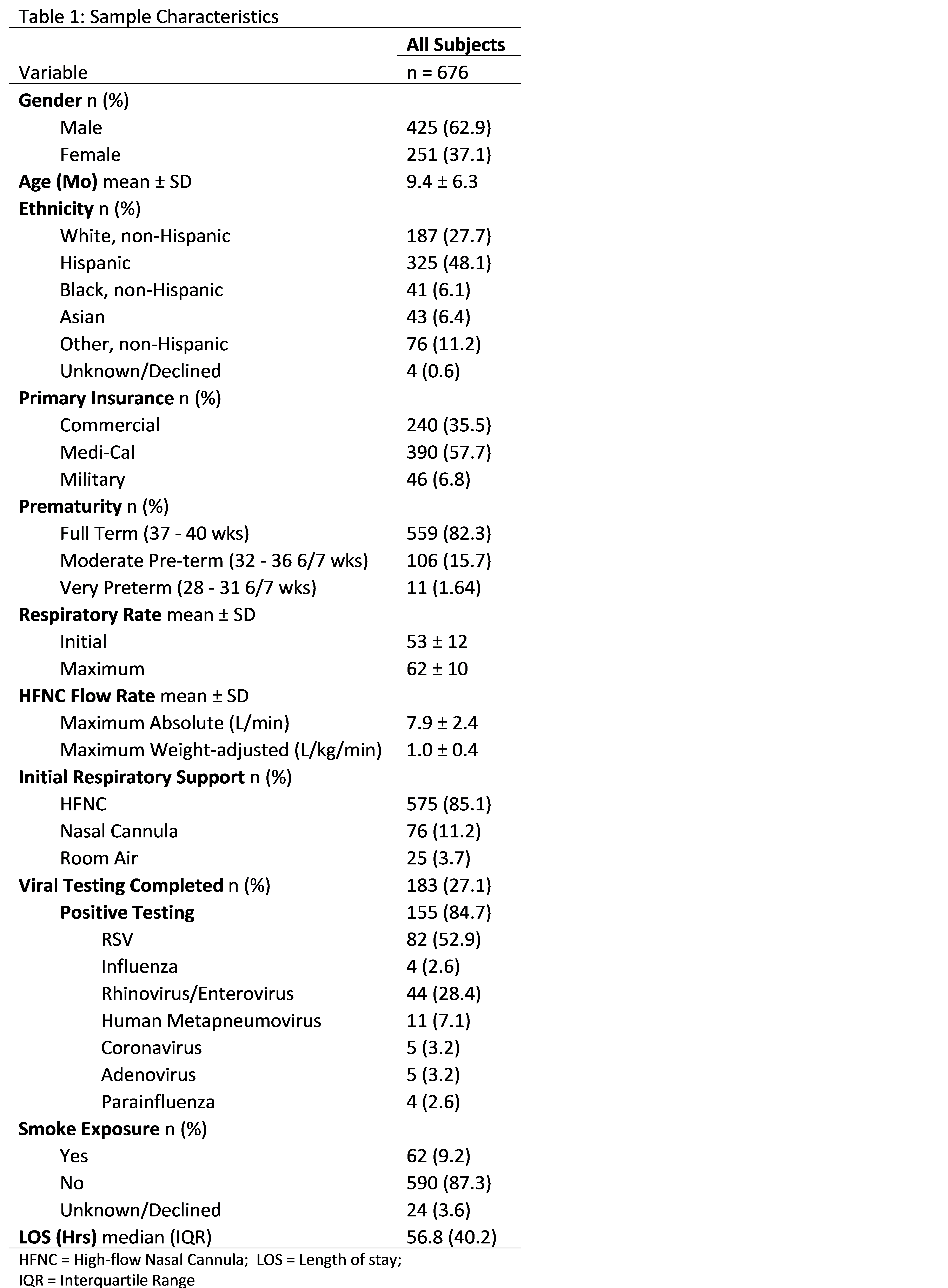
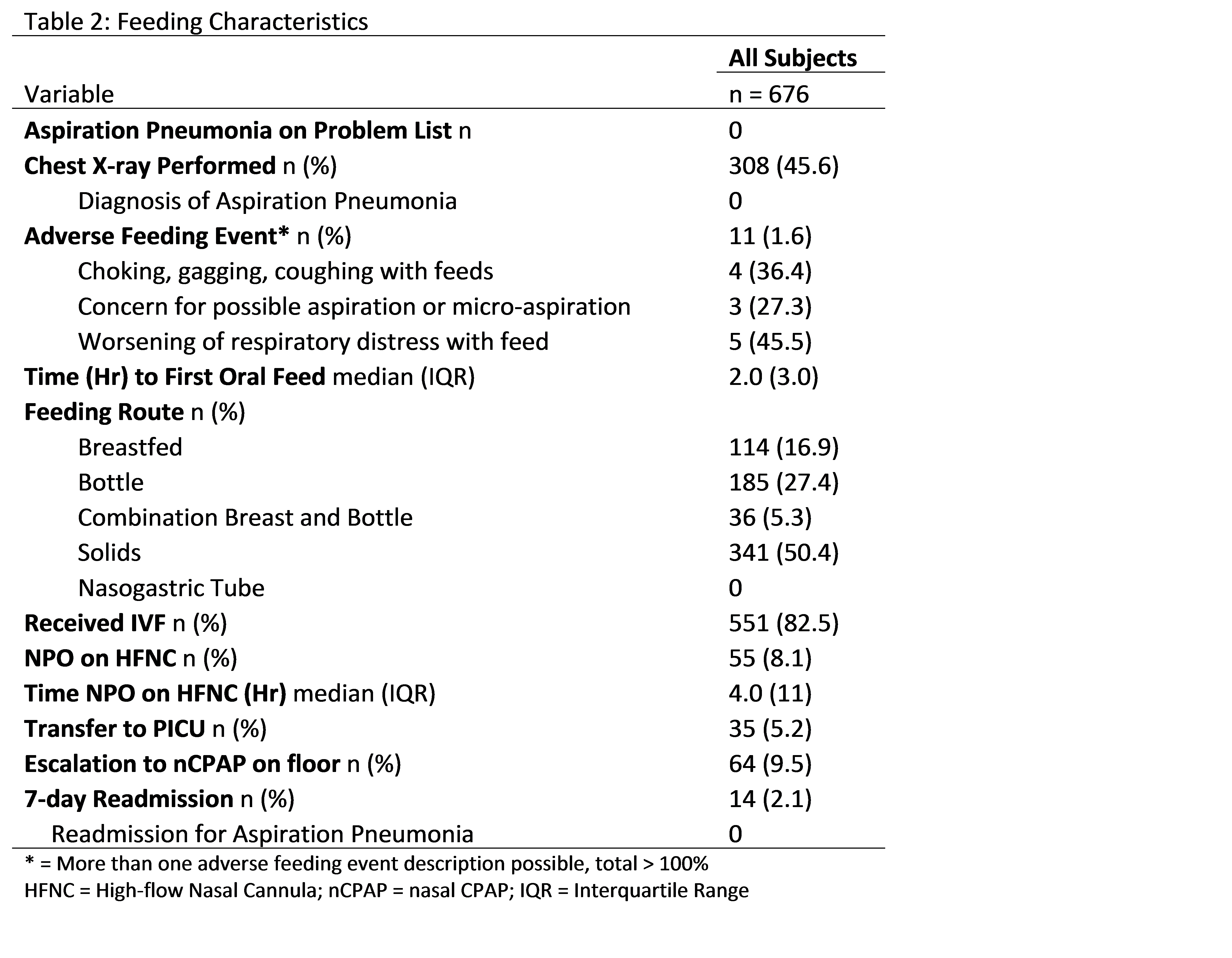
Results: Of the 876 patients with bronchiolitis on HFNC admitted to the pediatric ward, 676 met inclusion criteria. Sample characteristics are shown in Table 1. Adverse feeding events, such as choking or gagging with feeds, occurred in 11 patients (1.6%) (Table 2). Of those 11 patients, 3 had documentation concerning for possible micro-aspiration leading to increased respiratory support or LOS, but none were diagnosed with or received antibiotics for aspiration pneumonia. All patients received enteral nutrition by mouth and none by nasogastric tube, with a median time to first feed of 2 hours. The mean maximum HFNC flow rate was 7.9 L/min (weight-adjusted 1 L/kg/min). Escalation to nCPAP for worsening respiratory condition occurred in 64 patients (9.4%), and 35 patients (5.2%) transferred to the PICU. Patients were made NPO while on HFNC (n = 55, 8.1%) primarily due to worsening respiratory distress or prior to escalation in respiratory support, with a median time NPO of 4 hours. Patients who were made NPO during hospitalization were younger (6.4 vs. 9.7 months, p<0.001), had higher maximum respiratory rates (67.0 vs. 61.9, p<0.001), and had a longer LOS (103.6 vs. 60.7 hrs, p<0.001).
Conclusions: We identified a low incidence of adverse feeding events among children with bronchiolitis who were placed on HFNC and allowed to receive oral nutrition. No patients were diagnosed with aspiration pneumonia. Very few children were made NPO during the admission; those who were made NPO were more likely to be younger. These results suggest that adverse events related to feeding on HFNC are rare, and oral nutrition is well tolerated on this type of respiratory support.