Background: Effective mentorship of junior faculty correlates with future academic success and career sustainability.1,2 Traditional approaches to mentorship involve pairing mid- and late-career faculty with junior faculty randomly or based on compatible interests and allowing the relationship to evolve as driven by the mentee’s needs. After organized attempts to implement mentorship programs along traditional lines were unsuccessful, we sought to re-imagine our approach to match the evolving expectations and needs of the current generation of rising academic hospitalists, with an overarching goal of fostering academic success.
Purpose: We piloted a team-based, rapid cycle mentoring model with a primary aim of guiding hospitalists through turning an academic project into disseminated scholarly work and a secondary aim of identifying barriers and best practices to enhance future mentoring effectiveness and academic productivity in our group.
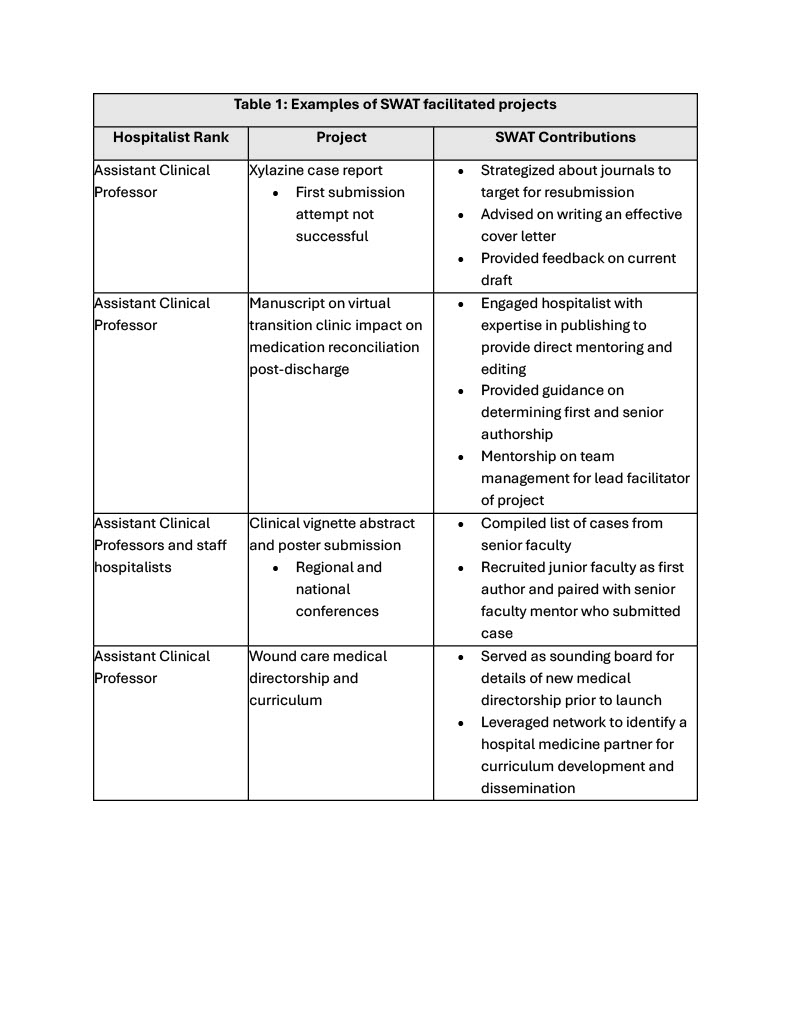
Description: We formed the Scholarly Work Activation Team (SWAT), comprised of five mid- to late-career Hospital Medicine faculty with expertise spanning medical education, quality improvement, publishing, health system operations, academic advancement, and mentoring. The team’s strategy is to curate time-limited mentor-mentee pairings around short-term, high-impact projects, and provide oversight and accountability via bi-weekly meetings. SWAT members leverage their networks across the academic and enterprise sectors to enhance project-specific collaboration. To assess the feasibility and effectiveness of this novel model, we invited individuals with an academic project in progress to participate in SWAT meetings. Table 1 lists the projects SWAT oversaw during the pilot period and the actions taken to move towards completion and dissemination. The SWAT team also identified hurdles and content gaps, which informed development of resources generalizable to our entire group. We plan to facilitate sessions on time management, best practices for mentees and mentors, and Lean Six Sigma training. Scholarship toolkits, including abstract and poster templates and best practice tips, a list of journals to target for publication, and a standardized process to obtain patient consent for case reports, were created and shared.
Conclusions: SWAT’s innovative approach to mentorship proved to be sustainable during the pilot period, and it was easy to identify hospitalists who were likely to benefit from participation. Regularly scheduled meetings and team-based mentoring helped participants make concrete steps towards project completion and allowed multi-dimensional coaching for junior faculty serving as project leaders. SWAT also inspired dissemination of resources intended to provide guidance and infrastructure to support the academic productivity of our entire group. Next steps include formally assessing the experience of SWAT participants and tracking scholarly activity and output to measure the effectiveness of this novel mentorship model.