Case Presentation: A 37-year-old man with a history of alcoholic cirrhosis and treated hepatitis C virus (HCV) infection as well as IV opioid use presented to the hospital with elevated liver function tests on intake labs at a substance abuse facility. Several years prior to presentation, he completed hepatitis C infection treatment with ledipasvir/sofosbuvir with sustained virologic response. He reported no alcohol or substance use in the prior week. His home medications included furosemide, spironolactone, citalopram, and buprenorphine. No fever, weight loss, excessive use of acetaminophen, salicylates, supplement use, nausea, vomiting, diarrhea, melena, jaundice, or hematemesis. He was afebrile and alert without asterixis. Abdomen was mildly distended but soft and nontender. Initial labs include AST 1,079 u/L, ALT 755 u/L, total bilirubin 3.7 mg/dL, INR 1.56, and alkaline phosphatase 14 IU/L, with a MELD score of 17. His liver function tests peaked at AST 1,826 u/L, ALT 1,622 u/L, and total bilirubin 23.2 mg/dL. Abdominal ultrasound was negative for thrombus or biliary obstruction. Alcohol level was negative. Urine toxicology was positive for cocaine, cannabis, buprenorphine, and fentanyl. HCV RNA viral load by PCR was greater than 2 million IU/mL. He was diagnosed with recurrent acute HCV infection causing severe acute liver injury (SALI). Cocaine-induced ischemic hepatitis was also considered, but less likely based on pattern of cocaine use and LFT trend. He was linked to outpatient treatment with sofosbuvir/velpatasvir as well as ongoing substance use treatment.
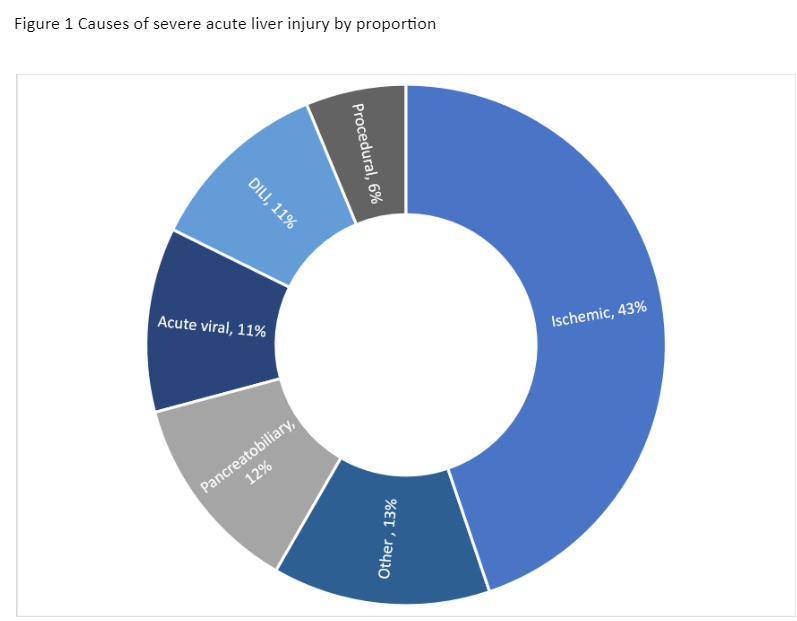
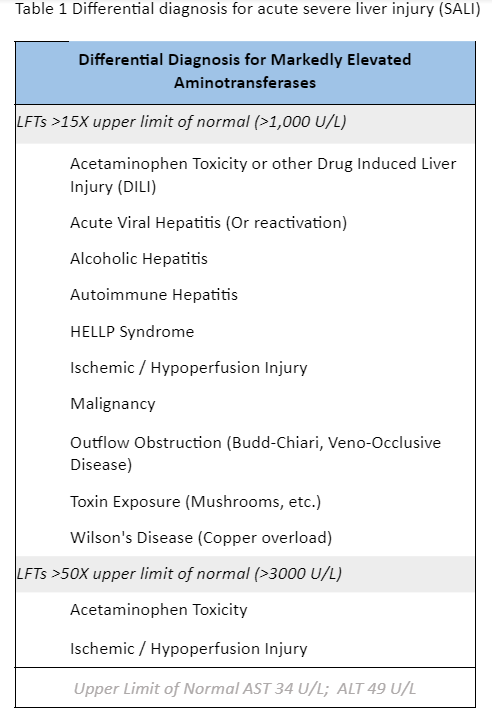
Discussion: Hospitalists should be familiar with the causes of SALI. SALI has various definitions but is commonly defined as AST or ALT >1,000 with acute onset of symptoms (< 26 weeks). Recognizing the etiology of SALI is important in management and prognosis (Table 1). The most common etiologies of SALI in a large, multi-site study in the US included ischemic hepatitis (42.7%), pancreatobiliary causes (12.3%), DILI (11.3%), and acute viral hepatitis (11.3%) (Figure 1)1. Although acute HCV was not strongly associated with severe liver injury in prior studies,2 in the above study it was responsible for 70% of viral causes of SALI (7% overall).1 In a retrospective UK cohort, HCV was the causative agent in 2.7% of total cases and about 22% of viral-induced cases.3 HCV antibody is not usually positive until 12 weeks after exposure, and thus is often negative in SALI due to acute hepatitis C.4 Additionally, HCV antibody remains positive even after treatment. PCR testing for HCV should thus be sent in SALI with prior infection or risk factors for HCV infection. While the overall five-year risk of reinfection after successful treatment for HCV is < 1%, the estimated 5-year reinfection rate in groups with high risk for HCV (persons with IV drug use, incarceration, or concurrent HIV) is between 10-15%.5-6
Conclusions: It is important to understand the most common etiologies of SALI and recognize HCV as a common viral cause of SALI in the US. HCV RNA PCR testing should be sent in patients with SALI and risk factors for HCV infection. Reinfection after successful treatment is rare overall, but is more common in certain higher risk groups, so should be considered if the patient has ongoing risk factors.