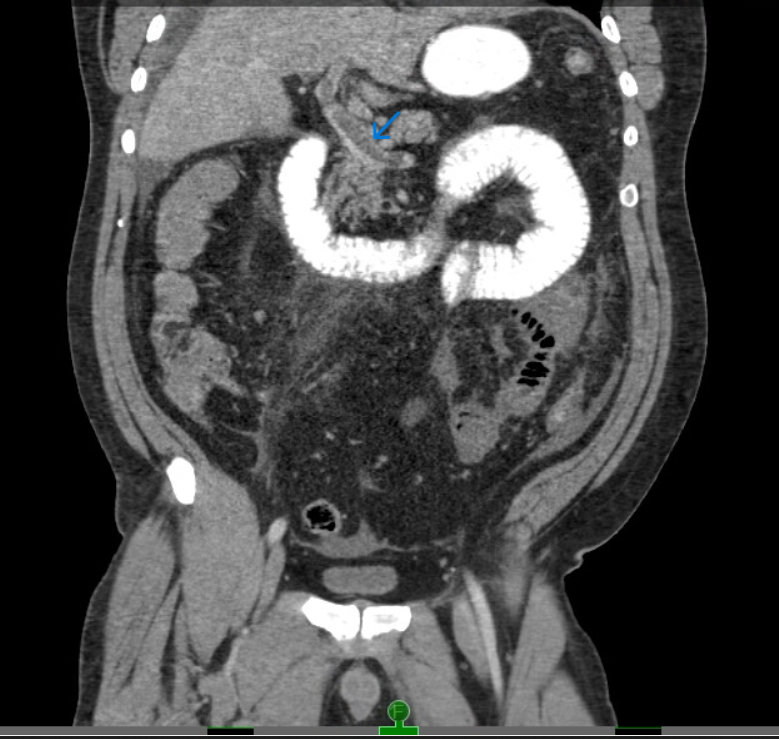
Case Presentation: A 52-year-old male with hypertension, sleep apnea, and polycythemia presented to an outside hospital for abdominal bloating and pain with emesis for 2 weeks. Labs showed WBC up to 26k/µl, AST of 166, ALT of 155, and total bilirubin of 2.8 mg/dl with normal range lipase and lactate. Initial CT abdomen pelvis (CTAP) showed concerns for enteritis, ileus, or partial obstruction. With his symptoms persisting, repeat CT found extensive portal venous thrombosis (PVT) extending to segmental branches and the superior mesenteric vein (SMV) involving loops of the mid and distal small bowel. His abdominal pain mostly resolved after broad antibiotics, heparin drip for PVT, and bowel decompression. Upon transfer to our hospital, his abdomen was nontender with mild distention on physical exam. Vascular and general surgery recommended conservative management, given his persistently normal lactate and benign exam. He remained stable with persistent bloating and intermittent food intake for several days. He then developed acute fever, with leukocyte count and total bilirubin rising to 37K/µl and 7mg/dl, respectively, despite only mild abdominal soreness on exam and unremarkable lactate. CT angiogram findings appeared mostly unchanged. Due to clinical deterioration, he underwent a laparoscopic procedure converted to open after encountering a dusky bowel with hemorrhagic exudate in the peritoneal cavity. Findings included 50cm of ischemic small bowel with hyperemic, thrombosed mesentery, and a frankly necrotic 15cm segment which was resected. The bowel was left in discontinuity, followed by an anastomosis 2 days later. Pathology showed acute ischemic enteritis with ulcerations and transmural necrosis. After the procedure, bilirubin, transaminase, leukocyte count, and abdominal distention improved. He tolerated a regular diet at discharge and on outpatient follow-up, recovered with regular bowel movements and resolution of pain.
Discussion: This report describes an unusual presentation of significant bowel necrosis, with persistently normal lactate levels, bloating, and only minimal abdominal tenderness on examination. Given his benign appearing presentation, surgery delayed intervention for nearly 10 days in the setting of a life-threatening condition. Although lactate typically increases in ischemia, in late presentations after necrosis, levels may have already risen and fallen to normal levels. Additionally, his normal lactate levels could stem from bowel necrosis due to venous thrombosis rather than artery thrombosis. Per literature review[1], portomesenteric system thrombosis is often initially misdiagnosed as a more benign condition due to milder symptoms when compared to acute artery bowel ischemia. The bowel infarction and necrosis process in venous thrombosis is also slower, consistent with our surgeon’s report that his necrosis appeared subacute over the course of weeks. This gradual nature can slow elevations in lactate, which may remain normal for a prolonged period.
Conclusions: In bowel necrosis secondary to portomesenteric system, the slow progression of thrombosis and bowel ischemia may lead to normal lactate and a benign exam[2], thus delaying lifesaving treatment. As a take-home note for hospitalists, normal lactate with persistently mild symptoms in a patient with PVT or mesenteric venous thrombosis does not rule out bowel necrosis. Furthermore, in patients with prolonged ischemia, late-stage necrosis may present with normal lactate.