Background: Approximately one-third of patients with acute ischemic stroke (AIS) develop hyperglycemia regardless of pre-existing history of diabetes [1]. Hyperglycemia is associated with increased risk of hemorrhagic transformation and can be considered as a predictor of poor functional outcome after intravenous thrombolysis (IVT) and mechanical thrombectomy (MT) [2]. Additionally, risk of death, hemorrhagic complications, and functional dependency are found to increase with stress-induced hyperglycemia especially in those without history of diabetes mellitus [3]. This study assesses whether stress-induced hyperglycemia is a predictor of poor outcome for patients with acute ischemic stroke (AIS) treated by endovascular treatment (EVT) and they are impacted by previous blood glucose status.
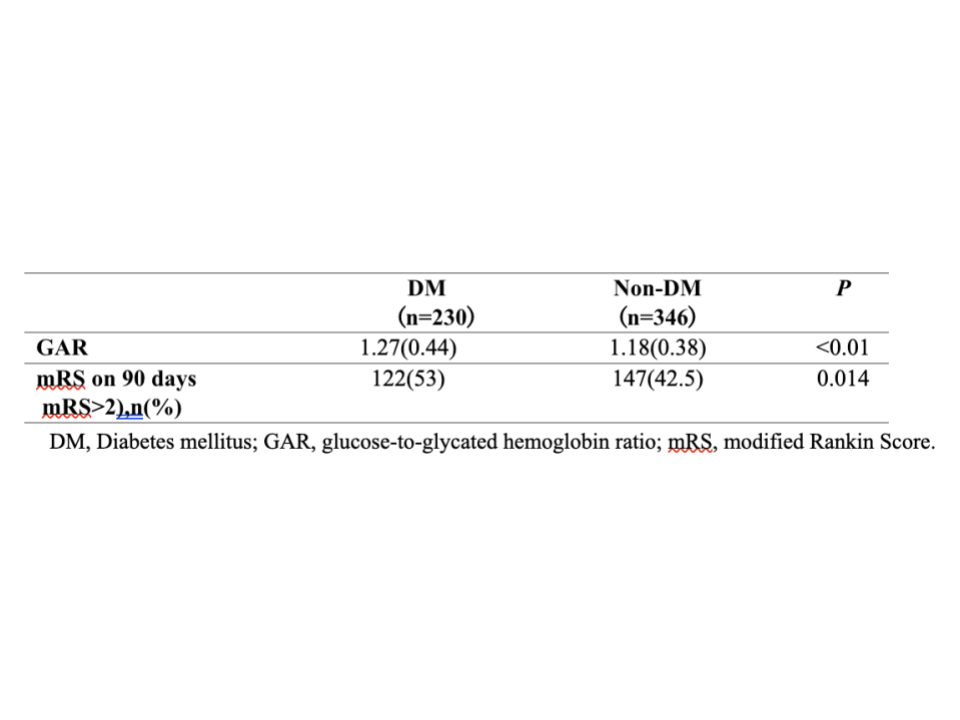
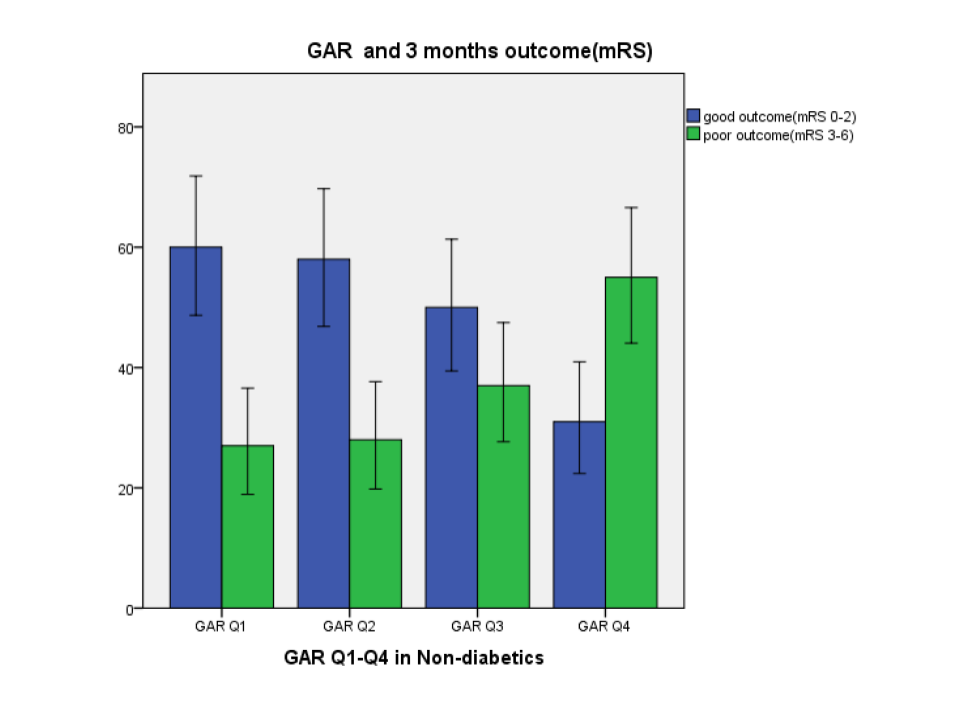
Methods: This retrospective study collected data from 576 patients with AIS of large vessel occlusion (LVO) treated by EVT from March 2019 to June 2022. The sample was composed of 230 and 346 patients with and without diabetes mellitus (DM), respectively, based on their premorbid diabetic status. Prognosis was assessed with modified Rankin Scale (mRS) score at 3-month after AIS. Poor prognosis was defined as mRS>2. Stress-induced hyperglycemia was assessed by fasting glucose-to-glycated hemoglobin ratio (GAR). Each group was stratified into 4 quartiles of GAR (Q1–Q4). Any significant association between stress-induced hyperglycemia and poor outcomes in both the DM and non-DM groups was assessed. Multivariate logistic regression analysis was used to identify any relationship between different GAR quartiles and clinical outcome after EVT.
Results: In DM group, poor prognosis was seen in 122 (53%) patients and GAR level was measured to be 1.27±0.44. These variables were higher than non-DM group and the differences were statistically significant (p< 0.05, respectively). Patients with more severe stress-induced hyperglycemia showed greater occurrence of poor prognosis at 3 months (in DM, Q1=39.7%, Q2=45.6%, Q3=58.6%, Q4=68.4%, p=0.009; in non-DM, Q1=31%, Q2=32.6%, Q3=42.5%, Q4=64%, p< 0.01). After logistic regression, the highest quartile of GAR was independently associated with 3-month poor outcome (OR 0.34, 95%CI 0.16-0.70, p=0.004).
Conclusions: The outcome of patients with LVO stroke treated with EVT appears to be influenced by premorbid diabetes status. However, the poor prognosis in diabetic patients is not independently associated with stress-induced hyperglycemia. This could be due to the long-term damage resulted from persistent hyperglycemia and/or the adaptive alterations of diabetic patients responding to stress-induced hepatic glucose metabolism after acute ischemic damage to the brain.