Background: Hospital discharge is a complex process for patients, caregivers, and providers. A robust understanding that the patient has regarding new diagnoses, medications, and appointments improves the capacity for self-care and post-discharge outcomes. The Team Discharge approach was successful at NYU Brooklyn Hospital and expanded to the Manhattan Campus
Purpose: To improve the patient experience of the discharge process by implementing a standardized nurse and provider touchpoint with patient before discharge to promote increased patient satisfaction with communication from the care team during the inpatient stay, with a goal of a positive correlation between nurse and provider joint rounding and HCAHPS top box responses.
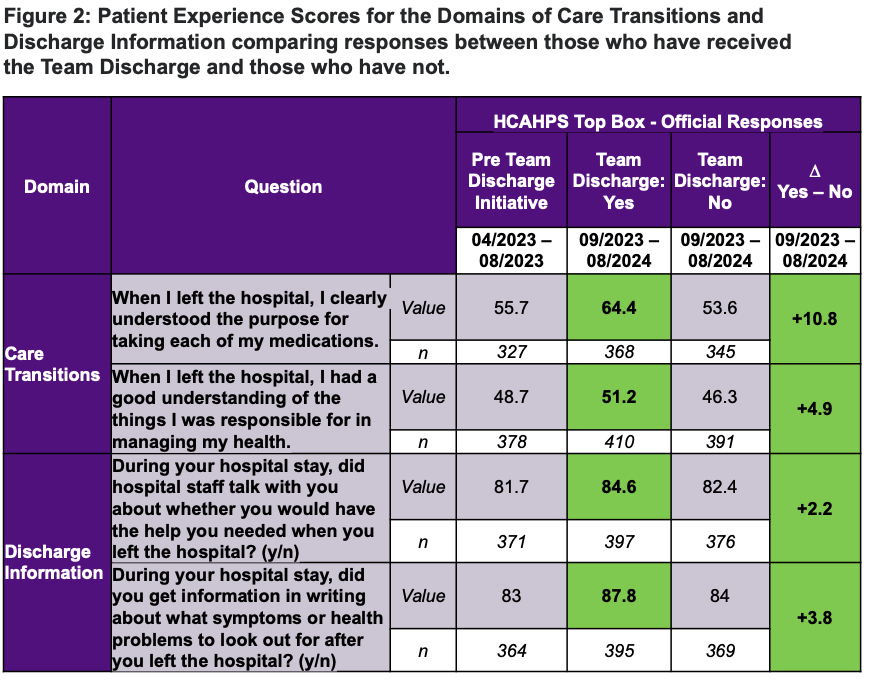
Description: The Medicine service implemented this Team Discharge starting in September 2023. Education of Team Discharge was messaged through monthly unit leadership meetings and weekly floor team meetings. Bedside nurses and providers utilized Epic secure chat to coordinate when to conduct the Team Discharge at the bedside. After the Team Discharge concluded, the bedside nurse entered an Epic Smartphrase into the patient’s chart to note completion. An Epic Workbench report was created to pull weekly and monthly compliance data to better understand the implementation of the Team Discharge (Figure 1). HCAHPS survey responses were linked to “Team Discharge completion” status, based on the presence or lack of a “Team Discharge” note during the encounter which was captured by the Epic Smartphrase. HCAHPS survey results from patients with a documented note of a completed Team Discharge were compared to patients without the intervention (Figure 2). Over the course of the year the compliance rate increased from 27% to 83%, an absolute increase of 56%. Two domains within the HCAHPs survey were analyzed, Care Transitions and Discharge Information. The most striking difference was observed for the question, “When I left the Hospital I clearly understood the purpose of taking each of my medications” with a 20% increase in top box scoring. In addition, there was an impressive 11% increase for the question, “When I left the hospital, I had a good understanding of the things I was responsible for managing my health”. Modest gains were achieved for the other questions that the Medicine service was already performing well in.
Conclusions: The Team Discharge provides an opportunity to bring the entire care team to the bedside at the time of discharge to explain and clarify discharge instructions to patients in a collaborative effort. Over the course of the fiscal year, there was significant improvement in the compliance of team discharge through multiple efforts. Using the Epic Workbench compliance reports, unit leadership was able to identify high and low performers on an individual basis as well as discover barriers and opportunities. Individual accountability along with unit and service-wide transparency rose the compliance 207% from the initiation in September through the end of August. Positive feedback was also received from the medical team members. The team discharge was felt to decrease Epic Secure chat use, improve medication accuracy, better highlight key points on the After Visit Summary, and overall increase the quality of the discharge. Team Discharge broke down barriers of the norm and instilled a culture change for the future of how we discharge patients.