Background: Readmissions continue to be a significant burden on health systems and in 2017 nearly 80% of all hospitals face financial penalties for 30-day readmissions. There are limited examples of standardized processes for notifying discharging physicians of readmissions real-time and encouraging physician self-reflection on reasons for readmissions.
Purpose: In the present study, we created a guided tool to notify Hospitalists of readmissions and to allow for review of the medical record, positing that awareness and reflection would lead to practice adjustments that would change overall readmission rates or change perspectives on the preventability and reasons for readmissions.
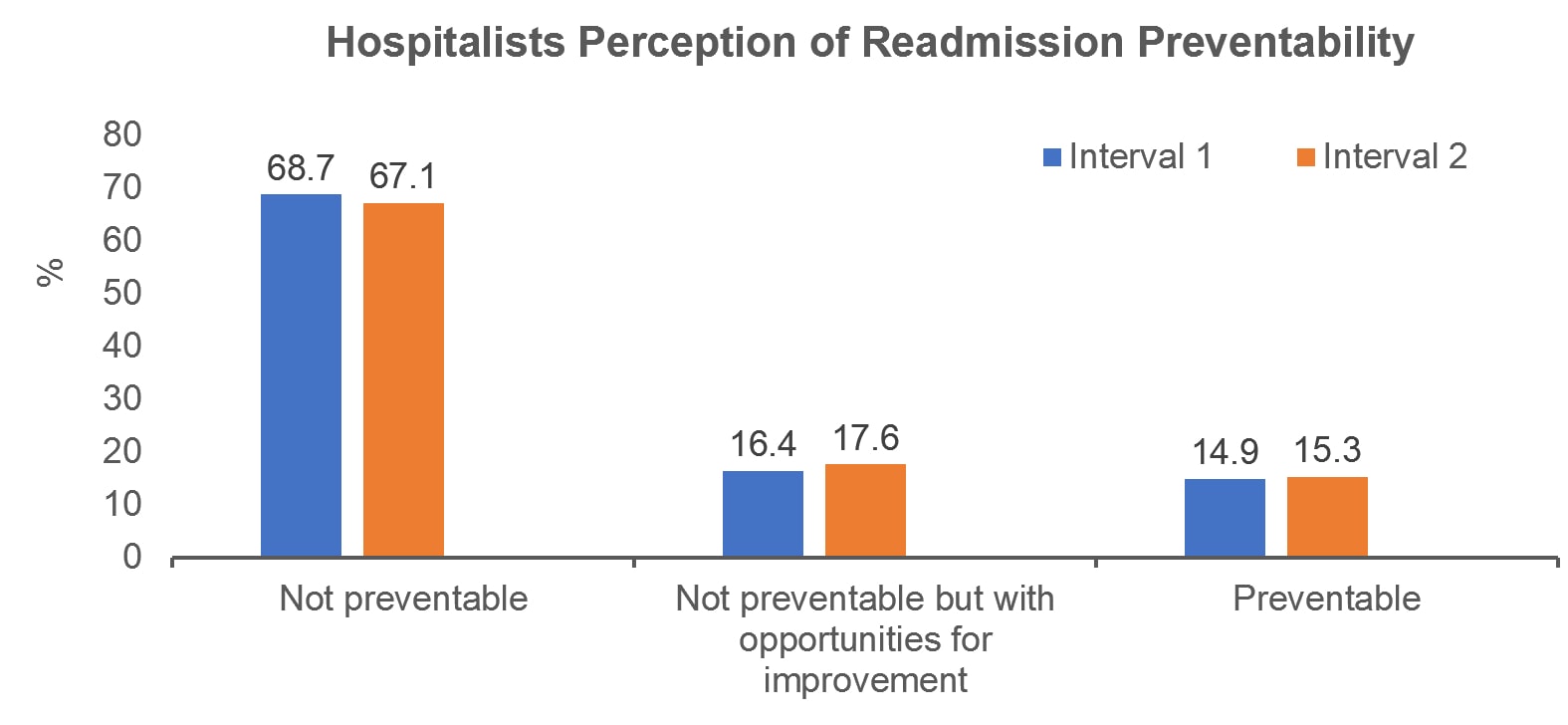
Description: From December 28, 2016 to November 21, 2017, we identified readmissions for patients discharged from the Hospitalist service (index admission) in the preceding 7-14 days. At the time of readmission the discharging physician from the index admission was sent a guided tool (questionnaire) that explored reasons for readmission, relationship to the index hospitalization, preventability, and potential prevention strategies. To assess for change in the perceptions of readmission preventability over time, the study period was split into two time periods (12/28/16-6/11/17 and 6/12/2017 – 11/21/2017). Chi-squared tests evaluated for statistically significant differences between the two time periods. Overall, 423 of 504 (83.9%) readmissions were reviewed and 37 (94.9%) hospitalists in the service reviewed at least one of their readmissions. Median age (IQR 25%, 75%) was 56 (42,69) years, with 195 (46%) male and 228 (53.9%) female, and a median time to readmission of 10 (8,12) days. One hundred and eighteen (27.9%) readmissions were identified as super-utilizers (≥5 hospitalizations per year). When examining the most common reasons for readmission, 288 (68.1%) were reported as “other”, of which 126 (68.5%) readmissions were reported primarily due to worsening symptoms. All other options, such as inadequate follow-up, inability to take medications, and social issues were reported in <10% of readmissions. Hospitalists reported 270 (64.6%) readmissions were related to the index admission, yet 287 (67.9%) readmissions were reported as not preventable. Prevention strategies were identified in 64 (15.3%) patients. In the first time interval, 201 readmissions occurred, whereas in the second 222 occurred. No significant differences between the first and second interval groups were seen in readmissions reported as “not preventable” (68.7% vs. 67.1%, p = 0.13).
Conclusions: Clinicians reported most readmissions were related to the index hospitalization and approximately two-thirds were reported not preventable, suggesting hospitalists struggle to identify how they can further reduce readmission rates. There was no statistically significant difference in the perception of readmission preventability between the time periods. Making providers cognizant of potential points of improvement was not enough to change readmission rates in our univariate analyses, suggesting interventions beyond provider self-reflection are needed to impact readmission rates.