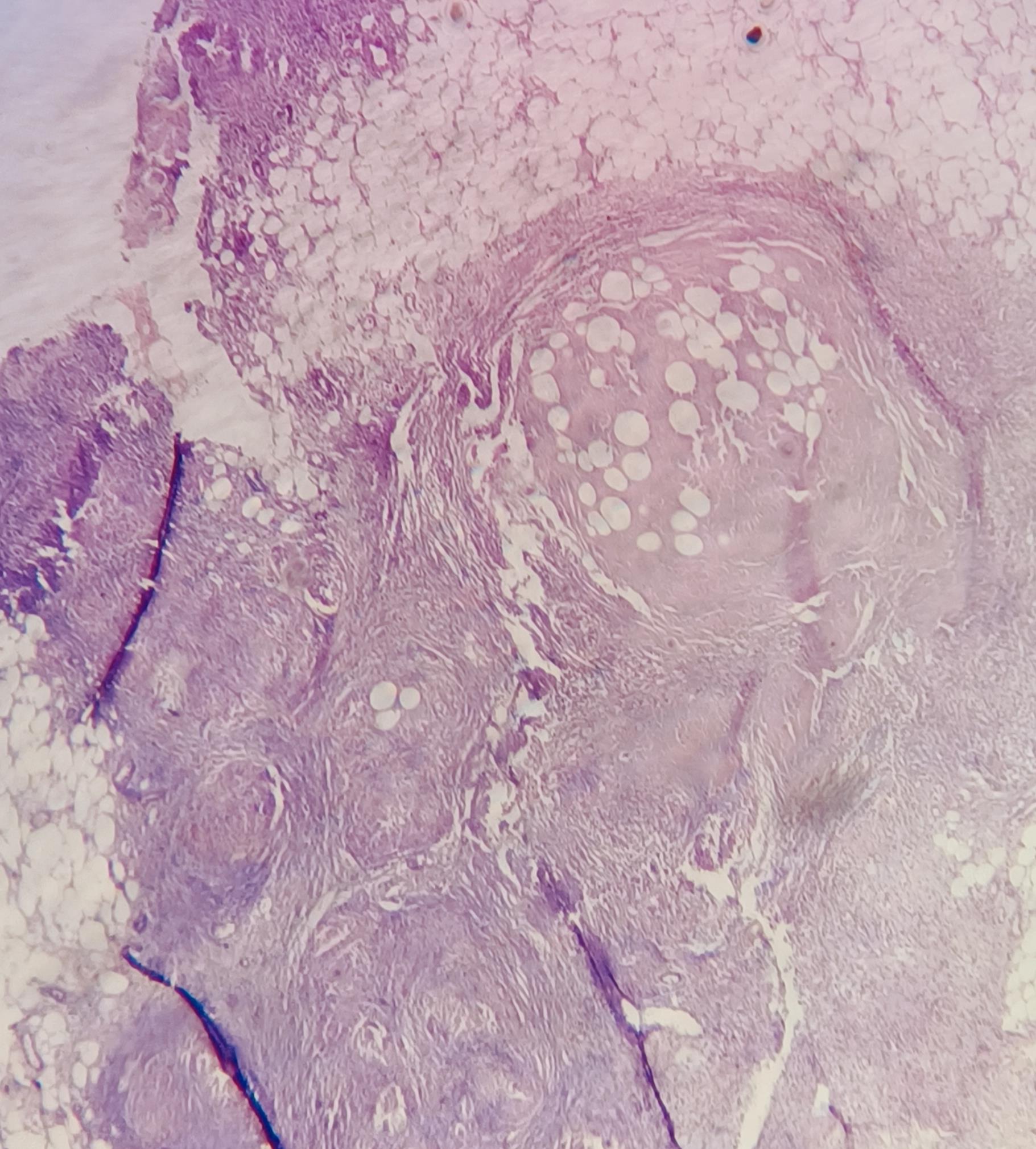
Case Presentation: Introduction:Tuberculosis (TB) remains a global health issue, with extrapulmonary TB often mimicking other conditions.¹ Diagnosing tuberculous peritonitis is particularly challenging in resource-limited settings, where nonspecific symptoms and limited diagnostics create barriers. This case highlights the complexities of diagnosing tuberculous peritonitis in a chronic alcoholic patient, initially suspected of decompensated liver disease (DCLD) despite negative TB tests.Case History:A 44-year-old male daily wage worker from Puducherry, India, with a history of chronic alcoholism, presented with three weeks of abdominal distension, two weeks of leg swelling, and unintentional weight loss. He denied fever, vomiting, jaundice, or urinary issues. He had no history of liver disease or TB and denied smoking, blood transfusions, and tattooing.Clinical Examination:The patient was conscious, thin, and poorly nourished, with bilateral Grade II pitting pedal edema and icterus. Vitals were stable. The abdomen was distended with shifting dullness, but no signs of liver failure. Palpation revealed a soft, non-tender abdomen with full flanks, no organomegaly, and present bowel sounds. Bilateral crepitations were noted on respiratory auscultation. Cardiovascular and neurological exams were normal.Provisional Diagnosis: Alcoholic decompensated liver disease (DCLD) without hepatic encephalopathy or spontaneous bacterial peritonitis.Management and Investigations:Initial labs, including CBC, RFT, coagulation profile, and urinalysis, were normal. ECG and ECHO were unremarkable, and LFT was within normal limits. Despite treatment for presumed DCLD, symptoms persisted. Ascitic fluid analysis revealed normal sugar, albumin, and protein levels but a low SAAG (0.8 mg/dL), significant lymphocytosis, and elevated ADA (51.5 IU/L), indicating a tuberculous or malignant etiology.CBNAAT and staining for Mycobacterium tuberculosis (MTB) were negative in ascitic and pleural fluid. Chest X-ray revealed right-sided pleural effusion. USG showed parenchymal liver disease. Despite negative staining, we ordered a CT abdomen which demonstrated gross ascites with omental stranding. Peritoneal and omental biopsy confirmed MTB on CBNAAT, and histopathology revealed caseating granulomas, consistent with tuberculous peritonitis. The patient was started on anti-tuberculous therapy (ATT) and discharged on day 15 after symptomatic improvement.
Discussion: Peritoneal tuberculosis can be challenging to diagnose due to its subacute nature and vague symptoms.² ³³ Our patient, initially treated as having chronic parenchymal liver disease at multiple hospitals, had refractory ascites and normal LFT, prompting further investigation and leading to the diagnosis of tuberculous peritonitis. Comorbidities like cirrhosis can mask the symptoms and lead to an atypical presentation, which may not prompt further investigation in common clinical practice.² ⁴ Hospitalists should carefully review patient records and adopt a multi-disciplinary approach in atypical cases to avoid delays in diagnosis and improve outcomes.
Conclusions: In parenchymal liver disease patients presenting with refractory ascites, always look for other causes of ascites. A high index of clinical suspicion, combined with invasive diagnostic methods and radiology, is crucial for identifying peritoneal tuberculosis in patients with atypical presentations and negative microbiological tests.