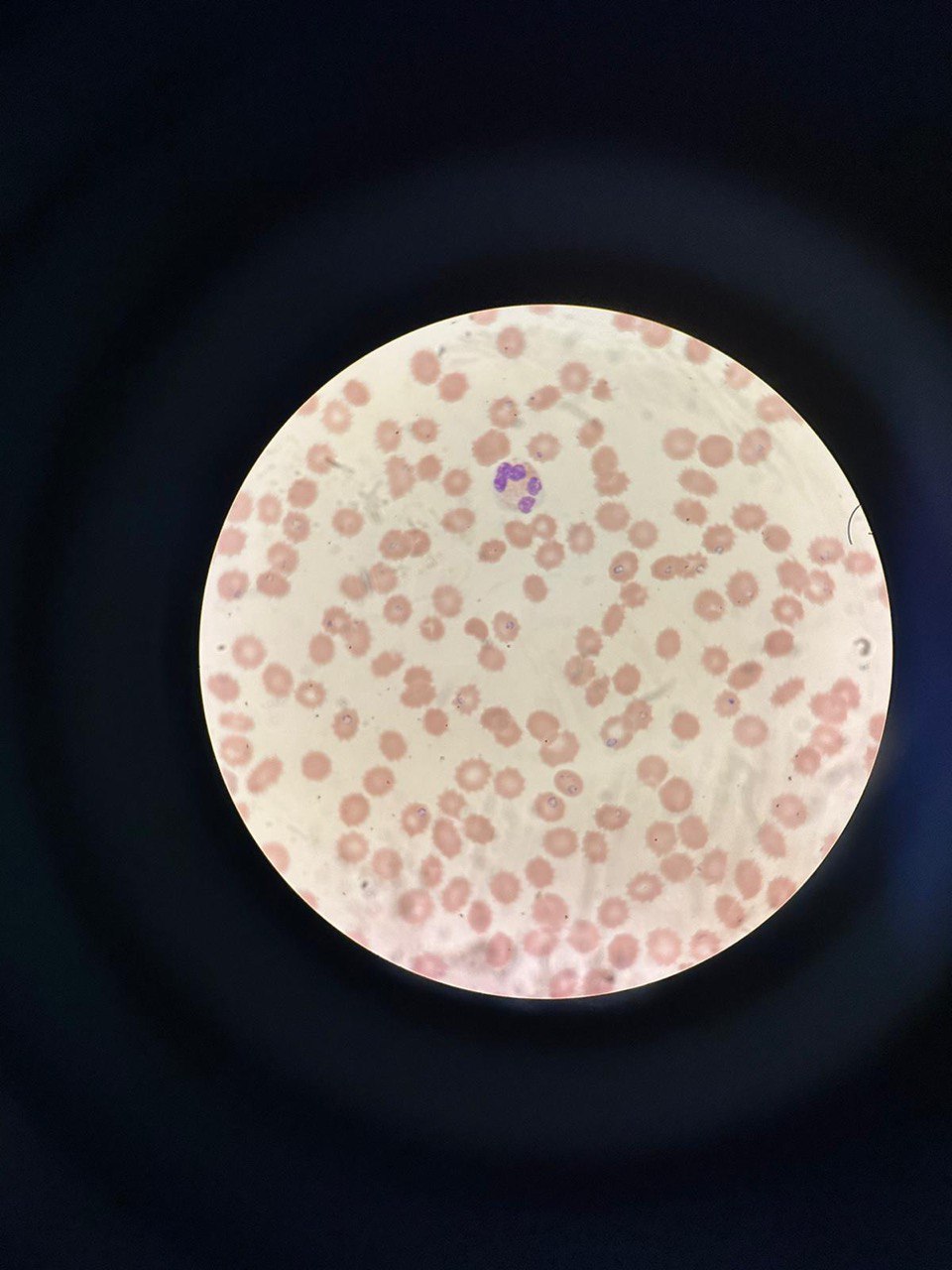
Case Presentation: A healthy 61-year-old woman residing in New York City presented with fever, fatigue, and decreased urinary output for four days. She was ill-appearing, jaundiced and hypotensive. Laboratory results were notable for WBC of 5.2/µl, hemoglobin 9 g/dl, platelet count 46,000/mm3, BUN 43 mg/dl, creatinine 4.36 g/dl, total bilirubin 4.6 mg/dl, direct bilirubin 1.5 mg/dl, reticulocytes 20%, LDH 16,570 U/L, and haptoglobin < 20 mg/dl. Direct Coombs test was negative. Patient was volume- resuscitated and started on broad-spectrum antibiotics. Peripheral blood smear was reviewed due to suspicion for thrombotic microangiopathy and instead revealed a large number of intraerythrocytic ring-forming parasites (parasite burden 22%). Given the patient’s history of recent travel to the Hamptons, we suspected babesiosis and started treatment with Azithromycin and Atovaquone. Despite treatment, the patient's blood pressure remained low, and her renal function deteriorated, necessitating vasopressors and hemodialysis. PCR ultimately confirmed Babesia microti. Follow-up peripheral smear three days after start of treatment showed parasite burden had decreased to 5%, and repeat testing at eight days was negative for parasites. Red blood cell exchange (RCE) was considered but deemed unnecessary due to steady reduction in parasitemia and clinical improvement. The patient was discharged 20 days after admission and on outpatient follow-up, she has had recovery of her renal function, though continued to have low-grade hemolysis.
Discussion: The incidence of babesiosis is rising [1]. Its presentation can range from asymptomatic to fulminant disease resulting in end-organ failure and death [2]. Disease severity correlates with parasite load and host’s immune status [3]. Diagnosis involves visualizing ring forms within red blood cells and using confirmatory PCR testing. Treatment primarily relies on antimicrobial therapy, with consideration of RCE in cases of high parasitemia (>10%), severe hemolysis, or end-organ failure. Combining RCE with antimicrobial therapy can rapidly reduce parasitemia and potentially improve outcomes [4,5]. Nevertheless, successful management of heavy parasitemia without RCE has been reported [6]. In our case, due to a significant drop in parasitemia from 22% to 5% within three days of initiating antimicrobial therapy, coupled with clinical improvement and reduction in hemolysis, RCE was not deemed necessary. It remains unclear whether RCE would have shortened the duration of hemolysis or reduced the length of stay.
Conclusions: This case underscores the need for a high clinical suspicion for babesiosis, especially in elderly individuals from endemic areas with febrile hemolytic anemia. Prompt peripheral blood smear review and early initiation of appropriate therapy is crucial in preventing potentially life-threatening complications. More research is needed to clarify the role of RCE in the management of severe babesiosis.