Background: Hospital reimbursement for medical necessity is based on the level of care a patient is receiving. In the electronic medical record (EMR), the level of care, inpatient or observation, is determined by a practitioner order or physician certification. The timeliness of this order is of utmost importance, as medical necessity is a dynamic status. In practice, a delay in changing the status order can result in a missed opportunity resulting in financial implications for the hospital, patient, and payor. Additionally, there are regulatory requirements for status orders. Failure to comply with these requirements can expose physicians and institutions to regulatory audits and allegations of fraud. Often practitioners are not well versed in the complicated medical necessity requirements that payors utilize, and they may rely on advice from a utilization review team regarding which status is most appropriate for a given circumstance. This communication between case managers and practitioners may be time intensive, impose on busy schedules, and risk delays in order status changes.
Methods: At our institution we developed an EMR-based workflow to improve the timeliness of status changes after concurrent reviews were performed for hospitalized patients. This workflow utilized an EMR-based concurrent review form populated by the case manager and physician advisor team. EMR logic compared utilization team recommendations with a patient’s existing care status. If a discordance was identified, a best practice advisory (BPA) was activated to alert the treatment team in real time. If the treatment team agreed with the recommendations, this BPA allowed order placement with fewer steps and minimized disruption to clinical workflow.
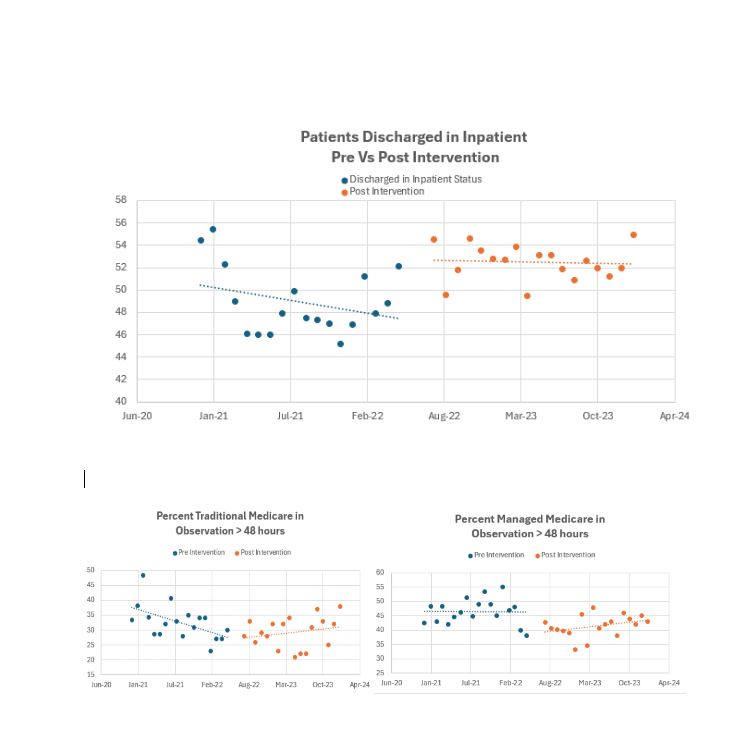
Results: The impact of the BPA was evaluated for 18 months before and after intervention. After implementation, case management status change recommendations using EMR-based BPAs resulted in provider responses in 68% of cases. Managed Medicare patients in observation status over 48 hours decreased from 46.5 +/- 4.5% pre-intervention to 41.5 +/- 3.8 % post-intervention (p = < 0.01), while traditional Medicare patients remaining in observation status for over 48 hours trended towards a decrease from 32.6 +/- 5.8% to 29.2 +/- 5.2% (p = 0.08). The number of patients discharged in inpatient status increased from 48.9 +/- 3.0% before the BPA to 52.5 +/- 1.6% after implementation (p < 0.01).
Conclusions: Our facility struggled with efficient communication and order changes for patient status. An EMR-based BPA improved the ease of communication and had an elevated level of practitioner participation(68% for our BPA as opposed to 20-30% of other BPAs in a report on response rates) resulting in a statistically significant decrease in managed Medicare patients in observation over 48 hours and an overall increase in the number of patients discharged in inpatient status. EMR based BPAs that facilitate communication are a potential solution for challenges and delays in case manager – practitioner communication.