Background: Since 2010, 130 rural hospitals have closed, leaving only 2,250 rural hospitals remaining in the United States. Of the remaining facilities, outmigration and/or the bypassing of the local hospitals to a larger facility remains problematic and impacts a community’s access to healthcare while affecting the long-term business viability of the city. In December of 2019, our academic medical center partnered to create a tele-hospitalist program with a rural, non-for-profit community hospital that had 85% of its residents receive their inpatient medical care outside their home facility
Purpose: To evaluate the impact of a tele-hospitalist program on a rural, non-for-profit hospital through reduction of outmigration. Key performance measures include average daily census (ADC), case-mix index (CMI), percent of ED patients admitted to the rural hospital, percent of inpatients transferred to an outside hospital, and 30-day readmission rate.
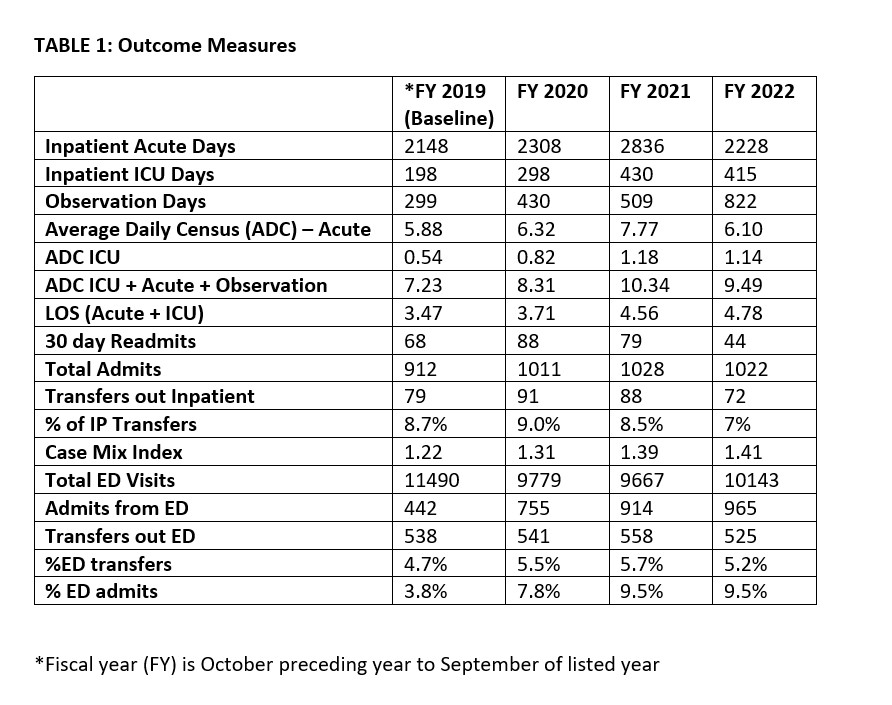
Description: Our tele-hospitalist program consists of hospitalists at a tertiary care academic medical center partnering with onsite advanced practice partners (APP) to provide coverage of all admitted patients at a small, 30 bed rural hospital. Tele-hospitalists are required to provide oversight to all new admissions daily via live tele-video conferencing encounters, and any additional patients at the discretion of the onsite APP. An observational study looking at all admissions at the rural hospital over a 3 year span was conducted. The pre-implementation fiscal year annual data was utilized for baseline data then annual reviews for the next 3 fiscal years were used for comparison. (Table 1)From the tele-hospitalist program inception in December 2019 through fiscal year 2022, the number of ED patients admitted to the rural hospital has increased from 442 patients per year (4%) to 965 patients per year (10%). Additionally, the number of ICU days has increased from 198 to 415 while the percent of inpatient transfers to an outside facility has decreased from 10% to 7% and the CMI has increased from 1.22 to 1.41. This demonstrates the ability to keep “sicker” patients locally. Of note, length of stay increased from 3.47 days to 4.78 days during this time period. As a result of this program, there has been a 24% increase in the average daily census from 2019 to 2022 (including inpatient, ICU and observation). Post-discharge, the number of 30-day readmissions has decreased from 68 in 2019 to 44 in 2022 (Table 1). Perhaps, most noteworthy, tele-hospitalists were able to support the hospital and local residents during the COVID-19 pandemic all the while receiving positive reviews from staff and residents.
Conclusions: Implementation of a tele-hospitalist program to a small, rural, non-for-profit hospital has increased the percentage of inpatients managed locally and, in doing so, improves access to care in rural communities without sacrificing quality as evidence by various outcome measures. This successful tele-hospitalist model serves as a template for viability for rural market hospitals and expansion to other critical access locations in the state is planned for the near future.