Background: Transitions of care are known to be high-risk times in healthcare, largely due to communication errors between providers. Prior studies have shown a direct relationship between poor signout practices and adverse events. Verbal handoff tools, such as I-PASS, have been created in efforts to facilitate the signout process. An important aspect of the handoff process is the written signout. While several studies demonstrate the efficacy of I-PASS as a verbal handoff, few have examined I-PASS explicitly as a written signout tool.
Purpose: The purpose of this study was to implement a written daily signout tool on a resident teaching service based on I-PASS and assess the quality, utilizing resident survey data as well as faculty evaluation guided by published rubrics.
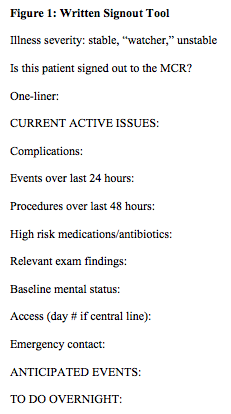
Description: The study was conducted among internal medicine housestaff on hospitalist teaching teams from November 2016 to November 2017 at a large urban academic hospital. The initial framework for the written signout incorporated the I-PASS elements. Using the Plan-Do-Study-Act (PDSA) cycle quality improvement process, modifications were added to the written signout tool for local hospital needs. Through resident focus groups and direct observations of the daily handoff process, additional elements were added to the written signout template (Figure 1).
Anonymous surveys were administered to residents to measure perceived quality of signouts, with 58 housestaff respondents prior to the implementation of I-PASS and 38 respondents afterwards. Prior to I-PASS, only 53.33% of residents agreed that the written signout identified active clinical issues, as compared to 100.00% afterwards (p=0.000). Similarly, only 26.67% agreed that the written signout identified the sickest patients prior to implementation, as compared to 91.17% afterwards (p=0.000). Additionally, agreement that the written signout provided anticipatory guidance for expected overnight clinical tests rose from 66.67% to 91.18% (p=0.009). Residents also felt the I-PASS tool was faster to complete with 90.91% of residents reporting that they spent less than 10 minutes completing written signout for a new patient using I-PASS, compared to 46.51% previously (p=0.000). Finally, overall satisfaction with the written signout tool rose from 27.91% to 96.97% after implementation (p=0.000).
Two hospitalist attendings evaluated the written signouts based on two published rubrics, the “UPDATED approach” and the “Faculty” scale, with scores 7 and above on both scales indicating superior signouts. Average UPDATED approach score rose from 6.5 to 8.4 (p=0.000) by one reviewer and from 5.5 to 7.6 (p=0.000) from the other reviewer after implantation of the I-PASS. Similarly, Faculty scale scores rose from 5.9 to 7.3 (p=0.038) from one reviewer and 7.1 to 8.1 (p=0.003) from the other reviewer after implementation.
Conclusions: Implementation of a written signout tool that incorporated the elements of I-PASS resulted in multiple areas of improvement, including anticipatory guidance and the identification of sick patients. Moreover, residents found the I-PASS tool faster to complete than the previous signout tool and had higher overall satisfaction. Faculty evaluation of written signouts also demonstrated increased completeness of written signouts after the adoption of I-PASS.