Case Presentation: 60-year-old woman with a twelve-year history of presumed gastroparesis of unclear etiology, was admitted for worsening chronic abdominal pain, nausea and vomiting with unintentional weight loss of over 80 pounds over a year. Evaluation included normal laboratory findings and abdominal imaging. Upper endoscopy showed mild mucosal erythema with normal biopsies of the stomach.
On hospital day 7, while awaiting a manometry rumination study, she became hypotensive. On exam, she was disoriented with new oculomotor dysfunction, slurred speech and ataxia. Laboratory analysis was significant for leukocytosis of 15.9 K/uL (normal 4.0-10.0 K/uL) and metabolic acidosis with a lactate of 5.9 mmol/L (normal 0.5-2.2 mmol/l). She was started on intravenous fluids and broad-spectrum antibiotics for presumed sepsis. Urinalysis was non-revealing and blood cultures were drawn. Cerebrospinal fluid analysis was significant for elevated protein of 313 (normal 15-60 mg/dl), 2 leukocytes (normal < 5 cells) and a negative gram stain. Hypotension improved, however patient remained encephalopathic and lactate rose to 6.2 mmol/L. Further work up with non-contrast head CT and MRI brain were negative for acute neurologic pathology.
Neurology recommended evaluation for seizures and treatment for presumed Wernicke-Korsakoff encephalopathy. EEG was negative for epileptic foci. Blood thiamine levels were drawn prior to administration of IV thiamine 500 mg three times a day for three days. With this treatment, patient’s mental status and ataxia resolved by day 9. Lactate normalized. Blood and CSF cultures remained negative and antibiotics were discontinued. Patient’s whole blood thiamine level returned at 37 nmol/L (normal 70-180 nmol/L) and serum thiamine was <7 nmol/L (normal 8-30 nmol/L). Her abdominal pain improved and she tolerated a soft diet without vomiting.
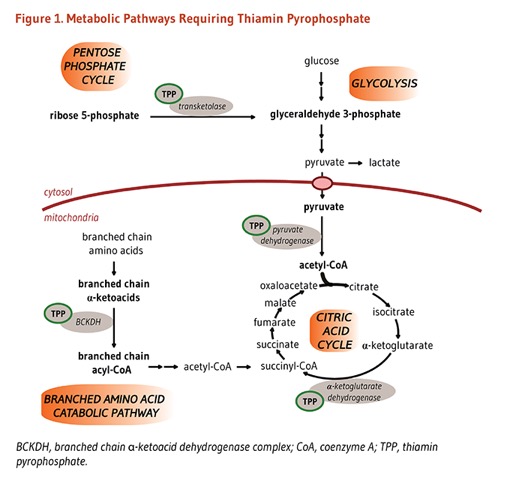
Discussion: Wernicke-Korsakoff syndrome is a clinical diagnosis of encephalopathy, nystagmus and ataxia, traditionally recognized in alcoholics but can occur in any patient with prolonged starvation. Administration of dextrose in thiamine deficiency, prevents the decarboxylation of glucose to acetyl-CoA in the Krebs cycle, resulting in metabolism of pyruvate to lactate. Several case reports have documented the occurrence of Gastrointestinal Beri-Beri from excess accumulation of lactate in patients with thiamine deficiency, presenting as abdominal pain, nausea and vomiting. These symptoms correct with administration of thiamine.
Conclusions: Hospitalists often care for patients with chronic abdominal pain and weight loss, thus it is important for them to recognize an unusual presentation of thiamine deficiency in a non-alcoholic patient. Furthermore, hospitalist should consider thiamine deficiency in the presence of unexplained metabolic acidosis, specifically, lactic acidosis.