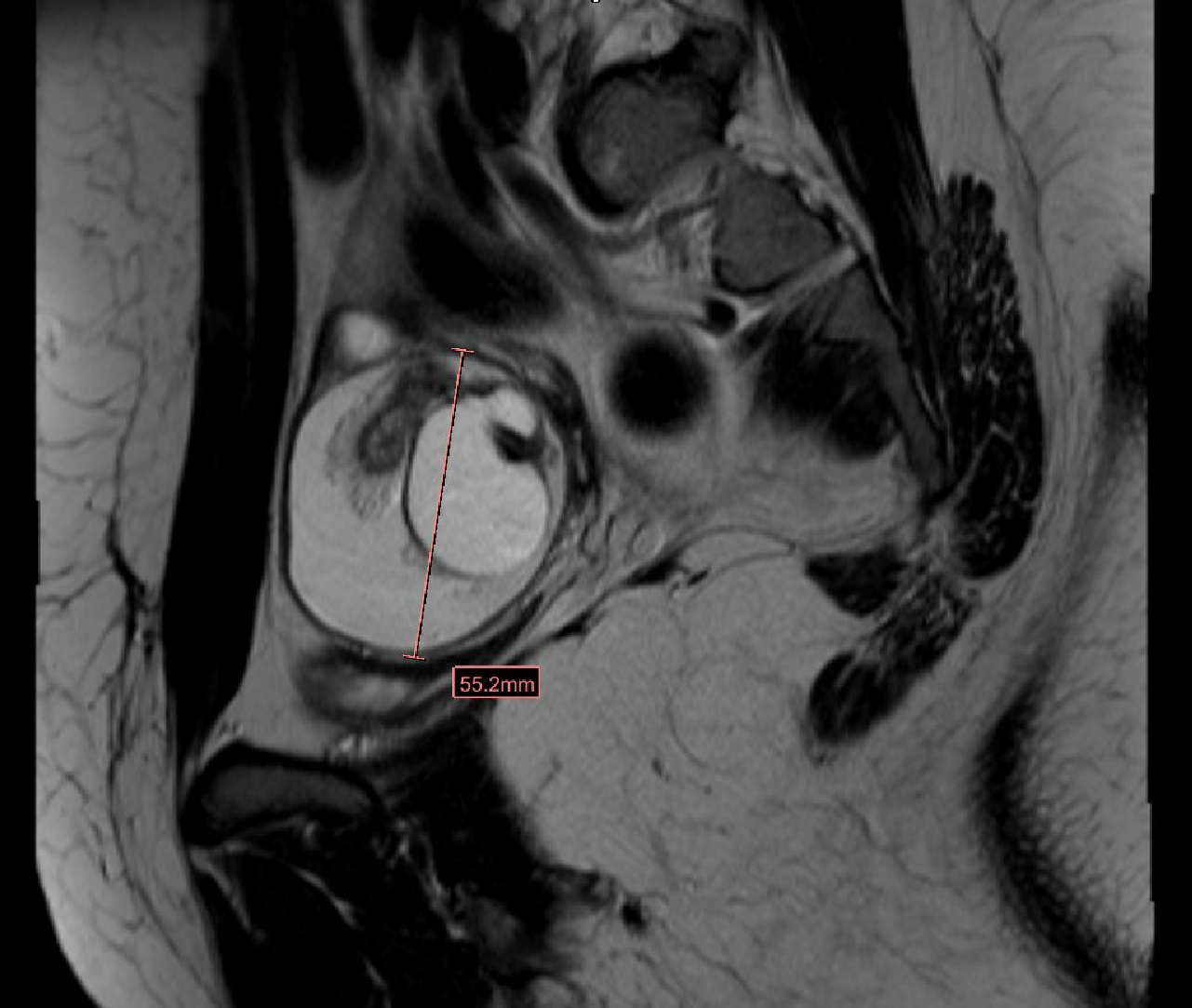
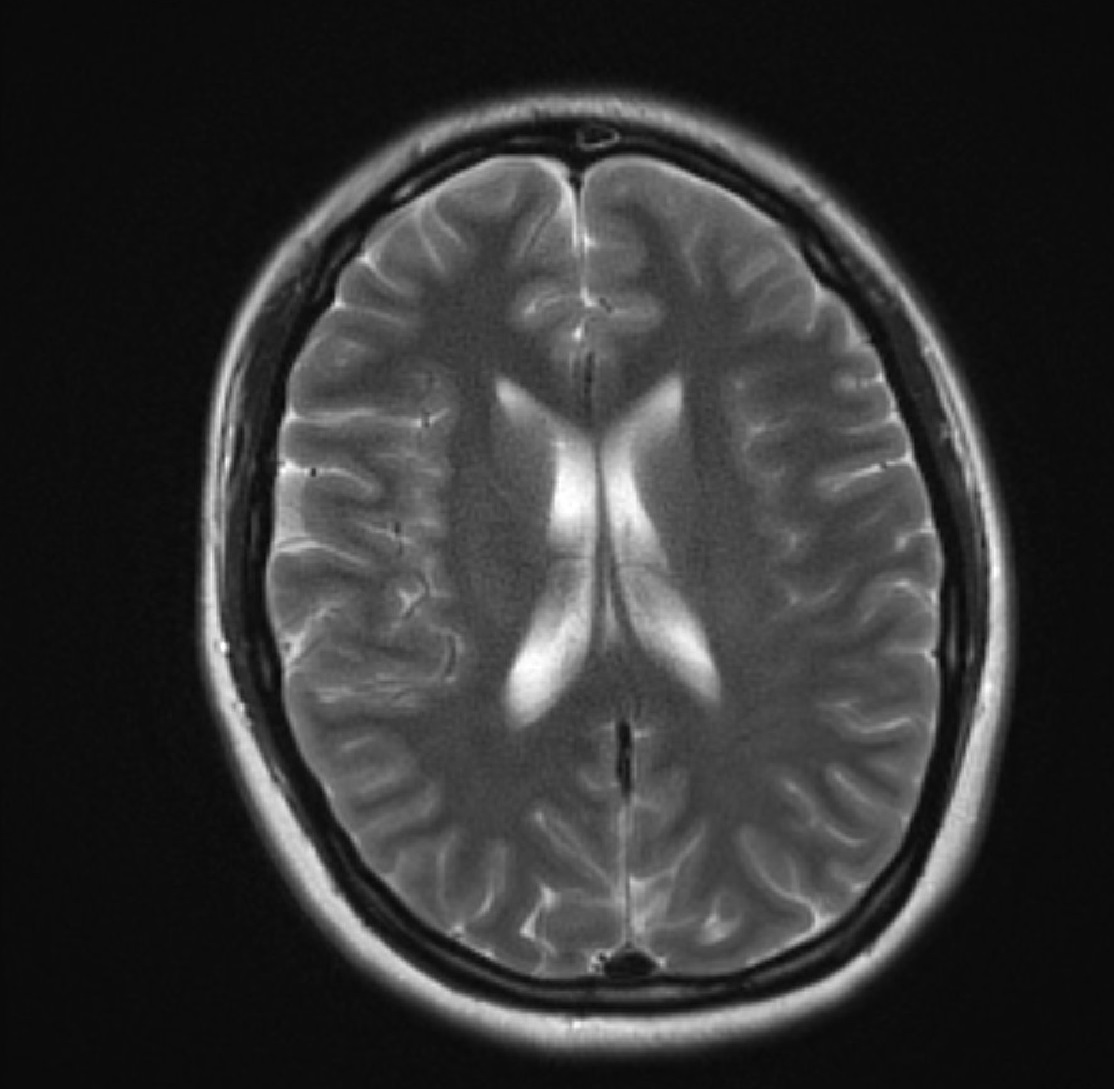
Case Presentation: An 18-year-old woman admitted to the hospital due to a new-onset tonic seizure lasting five minutes. She had recent history of flu-like illness a few weeks earlier. A review of systems revealed auditory and visual hallucinations. On physical examination, she was drowsy and disorientated to time only, but was following commands. Neurological examination showed an occasional myoclonic jerk and few beats of clonus bilaterally. Laboratory results showed normal hematology and biochemistry profile. Lumbar puncture revealed WBC 511/µl with 92% lymphocytosis, protein 28 mg/dl, glucose 97 mg/dl, and oligoclonal bands. Brain imaging was normal. The patient was started on empirical antibiotics and antiviral medications. Anyhow, she continued to deteriorate and became more lethargic, less communicative, with worsening involuntary movements. She was subsequently intubated and transferred to the Neuro-ICU. A 24-hour continuous EEG monitoring was negative for epileptic waveforms. Reassessment of the patient’s medical history revealed an undocumented history of right ovarian teratoma removal four years ago. Pelvic imaging showed left adnexal mass measuring 5.3x 4.5x 5.5 cm consistent with ovarian teratoma. Steroids and IV immunoglobulin were initiated for autoimmune encephalitis. Lumbar puncture was repeated and showed positive Anti-NMDA receptor (anti-gluN1) antibodies with a titer of 1:160, oligoclonal bands, and Anti-Myelin antibodies with a titer of 1:40. IgG index was high (0.77). The patient started to improve. Her seizures episodes subsided, and then she was extubated and transferred to the medical floor. Plans for surgical resection of the teratoma was arranged as an outpatient.
Discussion: NMDA (N- methyl-D-aspartate) receptors are ligand-gated cation channels, which are involved in synaptic transmission. Anti-NMDA receptor encephalitis is the most common form of autoimmune encephalitis, which is caused by an antibody production (often paraneoplastic) against NMDA receptors. Incidence is about 1.5 per million population per year. Female to male predominance ratio of around 8:2. Median age <21 years. The most common triggers are tumors (especially teratoma) and herpes simplex encephalitis. A viral prodrome usually precedes this syndrome. Clinical presentations include seizures, acute psychosis, movement disorders, and memory loss. Since its presentation is non-specific, thus high clinical suspicion should be considered for a constellation of movement disorder, seizures, and neuropsychiatric problems.CSF reveals lymphocytic pleocytosis, elevated protein, and oligoclonal bands. However, firm diagnosis is made by the detection of Anti-NMDA receptor antibodies in serum or CSF.Treatment is by tumor resection. It can also be treated with corticosteroids, plasmapheresis, and IV immunoglobulins. Patients without tumor, delayed diagnosis, or recurrent relapses of the disease might need rituximab, cyclophosphamide, or both.
Conclusions: Unexplained new-onset epilepsy in young women and adolescents may be a feature of anti-NMDAR encephalitis. Teratoma is highly associated with its pathophysiology. This syndrome is sometimes misdiagnosed as a primary psychiatric disorder. Early diagnosis and treatment can lead to better recovery. Those patients might need a long term follow up and rehabilitation for any persistent behavioral disorder.