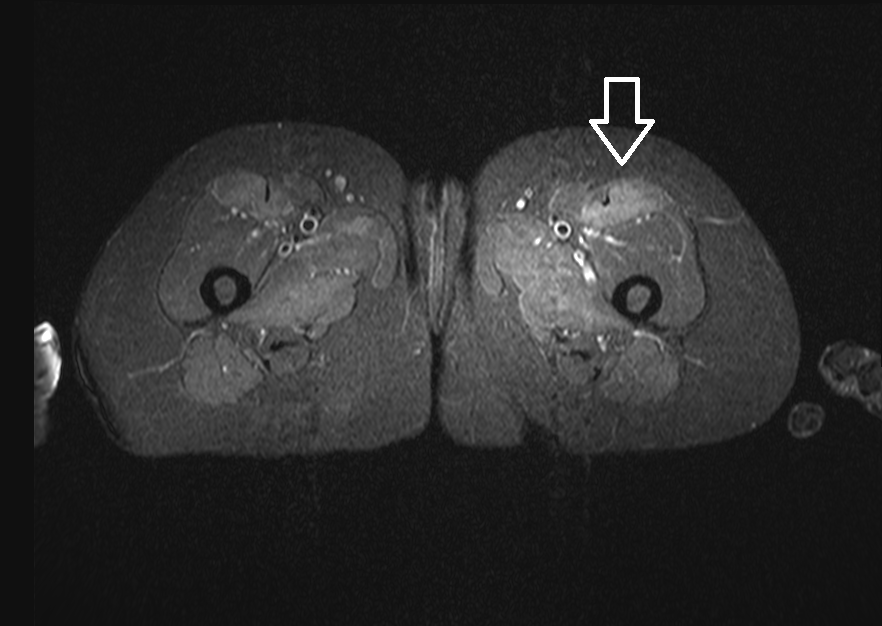
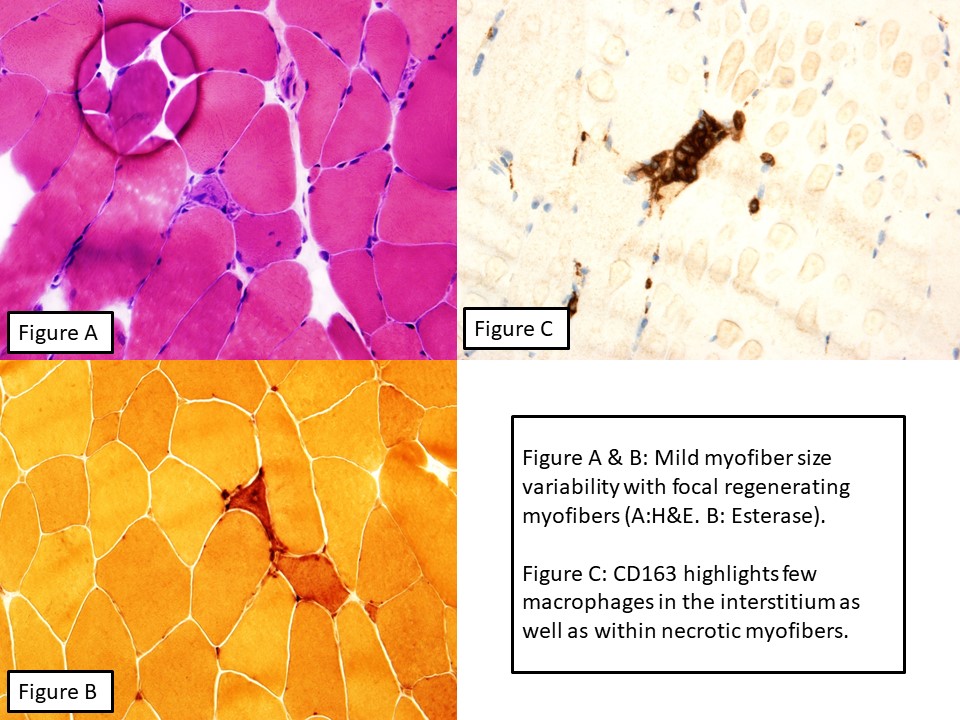
Case Presentation: Patient is a middle-aged African-American female with a history of hypertension and hyperlipidemia, for which she had been on atorvastatin for approximately four years. She originally presented to her primary care physician for evaluation of a one month history of progressive myalgias and proximal muscle weakness. Creatine phosphokinase (CPK) level was elevated to 18,000 and she was admitted to the hospital for IV hydration. Her atorvastatin was discontinued, CPK improved, and she was discharged. Upon hospital follow up, her CPK was found to be elevated with associated muscle symptoms, and patient was again admitted for IV hydration. Work up included unremarkable kidney, liver and thyroid function, a negative ANA, and negative antibody testing to smooth muscle, Liver-Kidney Microsomal, and mitochondria M2. Her Anti-HMGCR (3-hydroxy-3-methylglutyl-coenzyme A reductase) was positive. MRI showed intramuscular edema involving muscles of the shoulders, hips, thighs, and legs, and was most pronounced involving the left rectus femoris muscle. She underwent muscle biopsy from the left quadriceps which showed a mildly active necrotizing myopathy with myofiber necrosis, myophagocytosis and regeneration. She was diagnosed with Immune Mediated Necrotizing Myopathy (IMNM) and started on 60mg prednisone with taper over six weeks. Follow up as outpatient revealed improvement in her symptoms.
Discussion: As a result of their success in providing morbidity and mortality benefit from cardiovascular disease, statins have become one of the most widely prescribed medications worldwide. They are usually well tolerated, with myalgias being the most common side effect. This is normally self-limiting, however statin-induced necrotizing myositis is being increasingly recognized. Statin-induced autoimmune myositis is rare condition, with a prevalence of 1 in 100,000. Statin-induced myopathy is associated with the presence of autoantibodies directed against 3-hydroxy-3-methylglutaryl-coenzyme A. However, anti-HMGCR has a low positive predictive value and cannot be used alone to make the diagnosis. Proximal muscle weakness with marked serum creatine kinase elevations and histological evidence of myonecrosis, and with little or no inflammatory cell infiltration provide strong evidence for the condition. Response to treatment and long-term prognosis remain incompletely defined and the evidence for best-practice treatment is lacking. Based on case reports, steroids and methotrexate are a good initial therapy.
Conclusions: The pathogenesis of statin-induced autoimmune myositis remains unclear and due to the rarity of the condition, diagnosis can be challenging. A diagnosis of statin-induced autoimmune myositis can be considered likely in those statin-exposed patients who present with myalgias, muscle weakness, and elevated CK levels that test positive for anti-HMGCR antibodies. With increased reports of this condition, it may be possible in the future to risk stratify individuals for developing this complication prior to statin exposure and prevent unnecessary morbidity and mortality.