Background: As a result of COVID-19, clinical care across the U.S. has changed with virtual services becoming the new normal in many clinics.1-5 How these changes impact patient care following hospitalization is unclear as data are limited.6 We report on characteristics and rates of clinic follow up and satisfaction with care in patients discharged during the pandemic.
Methods: In this prospective cohort study, patients discharged from 23 hospitals across Michigan during the first COVID surge (3/14/2020 – 8/13/2020) were surveyed by phone 60 days following discharge. Eligible patients were identified from the MI-COVID19 database, a multi-institutional collaborative quality initiative, and included those hospitalized with or without COVID-19. Patients were excluded if they were <18 years-old, pregnant, left against medical advice, or were transitioned to comfort care within 3 hours of hospitalization. Patients at one site were also surveyed 30 to 40 days after discharge to assess satisfaction (on a 0-4 Likert scale) with their post-discharge care. We evaluated variation in hospital post-discharge method of care (e.g., video vs phone vs in-person) and compared follow up rates to previously-reported rates in the prior year at the same sites.7 Patient and hospital characteristics and patient satisfaction were assessed across visit formats. Chi-squared, Wilcoxon signed-rank, or t-tests were used to compare outcomes. P-value <.05 was considered statistically significant.
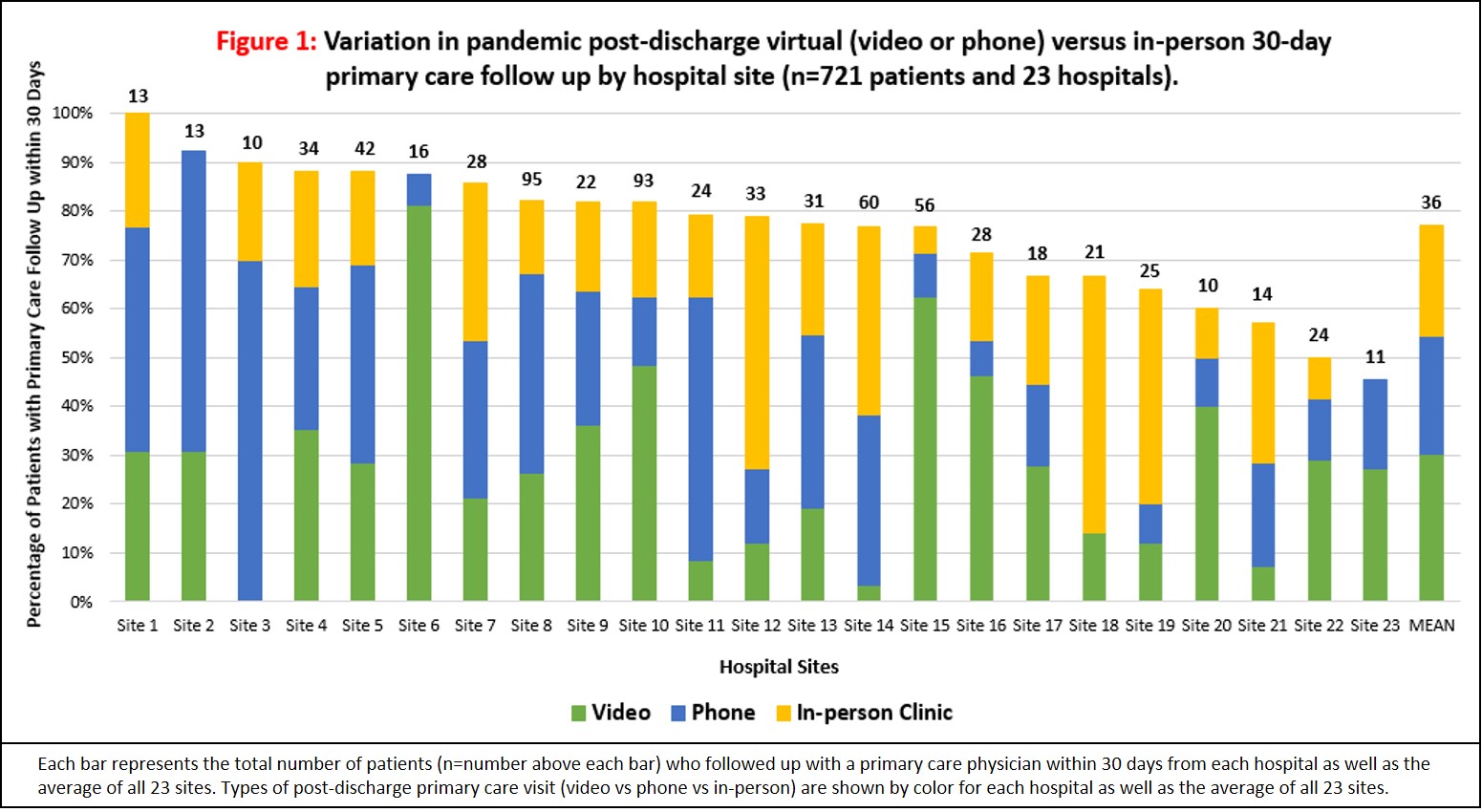
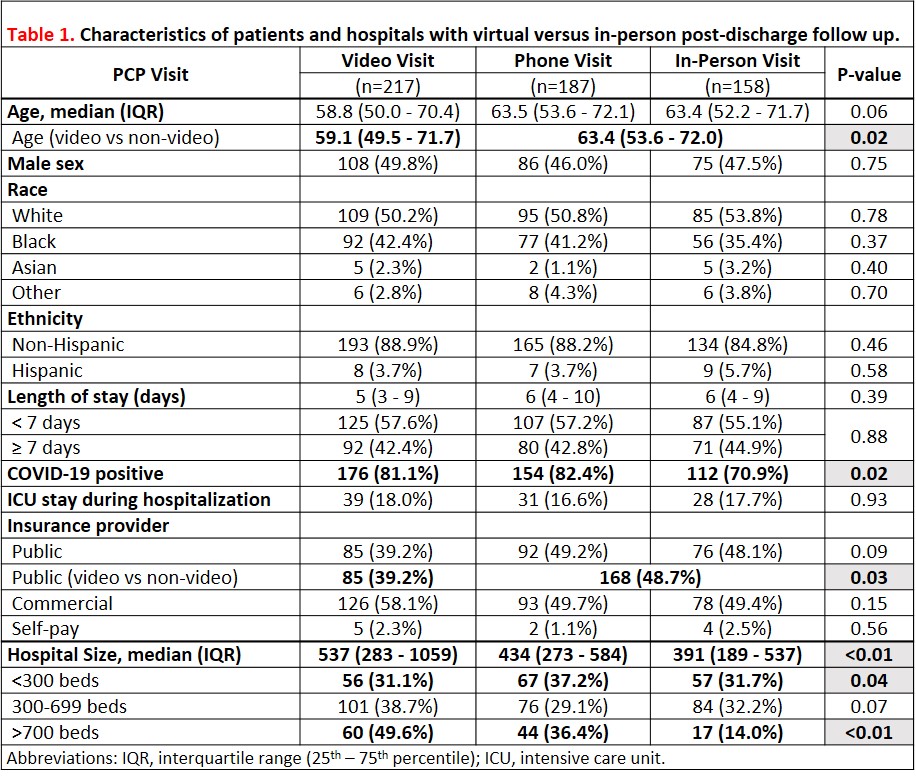
Results: Of 2,895 patients eligible for a 60-day phone survey, 721 were reached (response rate, 25%) and 561 (78%) were diagnosed with COVID-19 (Table 1). Three-fourths (78%, 562/721) of patients (with or without COVID) had followed up with a primary care provider within 30 days of discharge (range 45% to 100% across hospitals). Visit type varied: 29% were in-person, 32% by phone, and 39% by video. Across hospitals, use of virtual visits varied from 21% to 100% (Figure 1). Compared to the prior year, patients were more likely to have a post-discharge follow up visit during the pandemic (68% vs 37%, respectively, p=0.01). Patients with COVID-19 who had follow-up (N=442), were more likely to have virtual follow up (71% [112] in-person vs 82% [154] phone vs 81% [176] video, p=0.02). Younger patients were more likely to use video visits (median [IQR] age, 59 [49-71]) than non-video visits (63 [54-72], p=0.02). In contrast, patients with public insurance were more likely to use non-video visits (39% video vs 49% non-video, p=0.03). Larger hospital size correlated with use of video visits (50% [60/121] of patients from sites with ≥ 700 beds, 39% [101/261] from sites with 300-699 beds and 31% [56/180] from sites with < 300 beds, p=0.01). Of 192 patients assessed for satisfaction with post-discharge care, satisfaction was similar between visit types (mean satisfaction score [standard deviation], in-person 3.6 [0.7] vs phone 3.4 [1.0] vs video 3.5 [1.0], p=0.84).
Conclusions: During the COVID-19 pandemic, rates of post-discharge follow up were high. Virtual visits were commonly used, especially among COVID-19 patients and those discharged from larger hospitals. Video visits were more often utilized by younger patients and less often by those with public insurance, suggesting barriers to access. Transitioning to post-discharge virtual visits appears to potentially improve access to post-discharge care and is well-received by patients. With continued support by insurance payers, virtual care could be a novel strategy to improve post-discharge follow up.