Background: In 2013, the American Academy of Pediatrics’ position statement, “Guiding Principles for Pediatric Hospital Medicine (PHM) Programs,” emphasized the importance of professional development for each PHM physician. However, little is published about PHM physicians’ perspectives on professional development. The objectives of this study were to explore pediatric hospitalists’ perceptions of professional development needs, desired educational formats, barriers to and opportunities for engaging in professional development, as well as to develop a theoretical framework for professional development in PHM.
Methods: We conducted an IRB-approved qualitative study using 4 semi-structured focus groups in April-May 2019, with a separate focus group for division leadership. Questions were developed by expert consensus to address each study objective. Focus groups were audio-recorded and transcribed verbatim. Two investigators independently coded the transcripts and reconciled codes to develop themes using the constant comparative approach associated with grounded theory. Two additional authors reviewed all the code applications for validation. To further ensure trustworthiness, participants reviewed and commented on the themes’ accuracy.
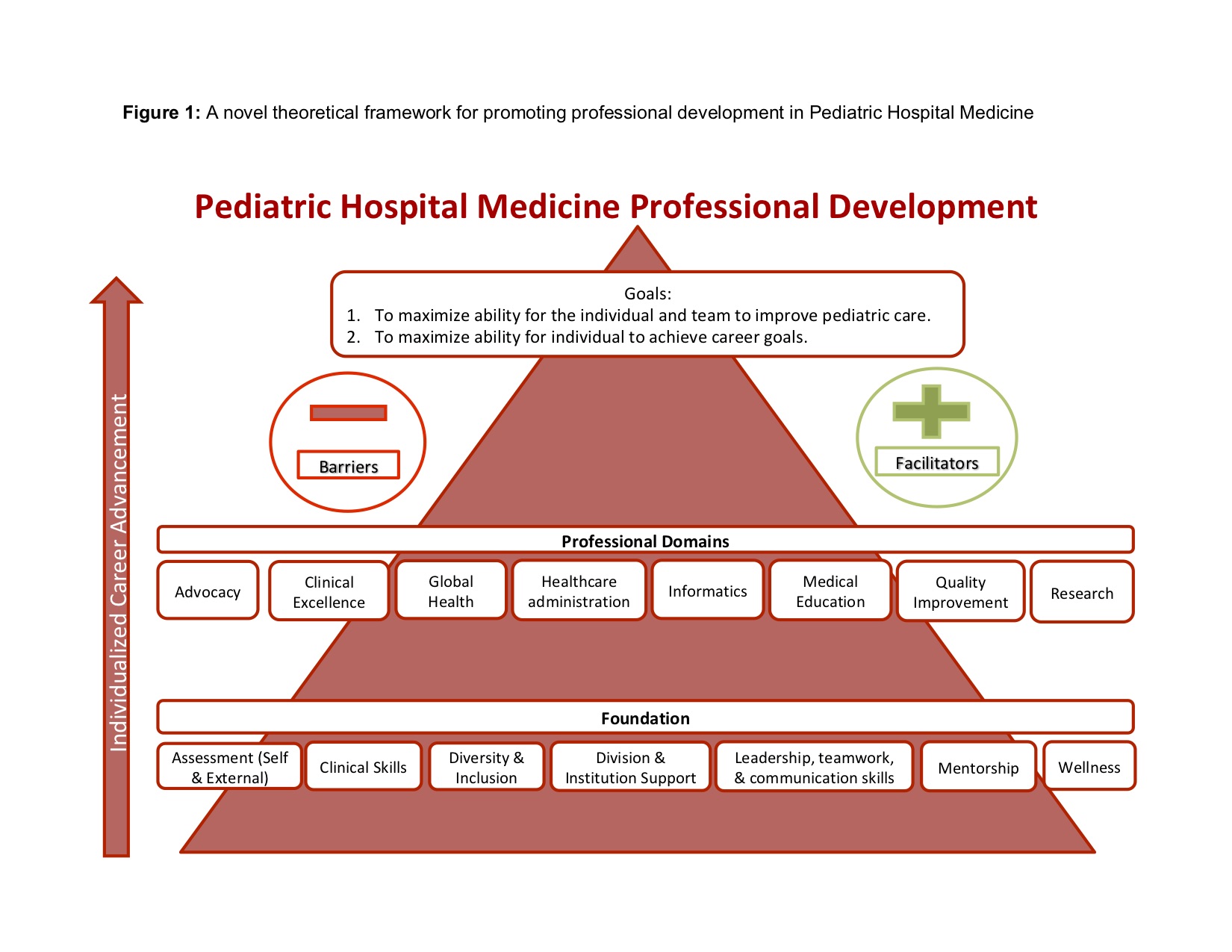
Results: 19 pediatric hospitalists at a large academic medical center and three regional community hospitals participated in focus groups. Five themes emerged: 1) Hospitalists identified key components of professional development including skill development, personal growth, career satisfaction, and individualization; 2) Hospitalists identified 8 areas of professional development within PHM: advocacy, clinical excellence, global health, healthcare administration, informatics, medical education, quality improvement, and research; 3) Hospitalists identified barriers and facilitating factors to participating in professional development; 4) Hospitalists validated missing the tools and mentorship to change their projects and passions into career advancement; and 5) The mutual benefit of aligning projects that are personally meaningful to what is meaningful to the institution.
Conclusions: Pediatric hospitalists felt the ultimate goals of professional development were to empower the individual and team to improve pediatric care and to maximize the ability of the individual to achieve career goals. In order to achieve these goals, PHM programs must build infrastructure that includes assessments of an individual’s skills; division/institution support of professional development; career mentorship; individual leadership, teamwork and communication skills; personal wellness; and strong clinical skills.