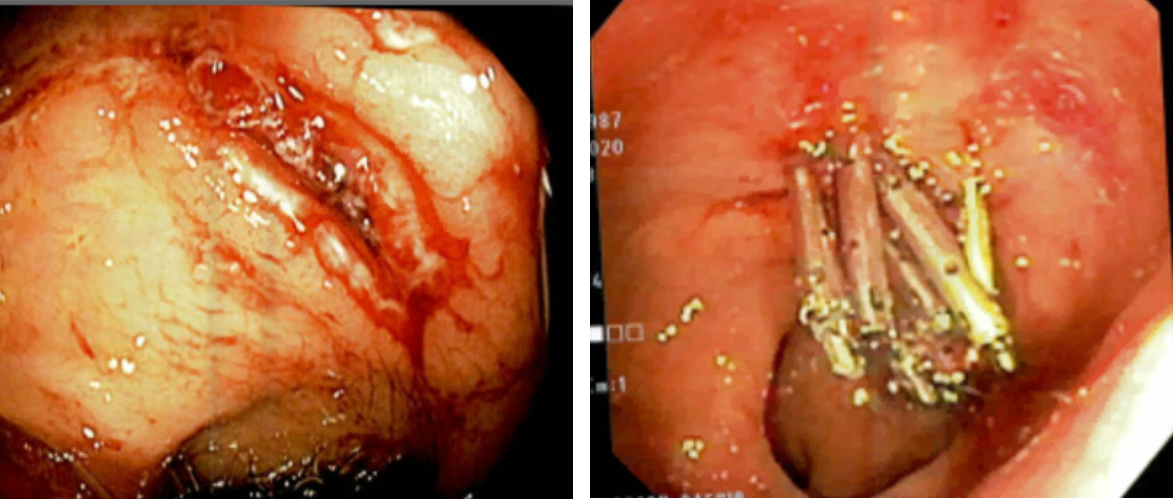
Case Presentation: A 33-year-old female was initially admitted to the ICU for septic shock secondary to complicated Pseudomonas aeruginosa urinary tract infection and methicillin-sensitive Staphylococcus aureus bacteremia. CT of the abdomen showed fluid in the left paracolic gutter. Aspiration and culture of the fluid was positive for Staph aureus and attributed to seeding from bacteremia. An incidental finding on the CT abdomen at admission was fatty liver, likely due to her chronic alcohol abuse. On day 10 of her hospitalization she developed altered mental status and, notably, had not had a bowel movement in 6 days. Ammonia level was elevated to 160 g/dL. Her altered mentation was attributed to hepatic encephalopathy. She was started on lactulose enemas with rectal tube placement due to concern of her ability to take medications safely by mouth. Several days following rectal tube insertion her mentation had improved to some degree when the patient then forcibly avulsed the inflated tube, leading to a large episode of hematochezia and hypotension. Sigmoidoscopy revealed a 2.5cm mucosal laceration in the rectum. Hemostasis was achieved with 5 clips and 10mL injection of 1:1,000 concentrate epinephrine. Repeat sigmoidoscopy was indicated 8 days later when the patient had another incident of hematochezia. This revealed an actively bleeding vessel within an ulcer at the site of previous injury, requiring an additional 5 clips.
Discussion: With the prevalence of fecal incontinence estimated to be as high as 50% in nursing home residents and up to 40% in intensive care units [1,2], this problem has led to an increased utilization of resources in both settings and decreased quality of life for patients. Whereas typical means of management include plastic sheets, incontinence pads, and frequent linen changes, rectal tubes are now commonly used in order to maintain a sanitary environment, prevent cross-contamination, and ensure skin integrity in the hospital setting.[3]A rectal tube works by sitting in the rectal vault and forms a seal allowing for the collection of any liquid stool. Because of its location and mechanism, the tube applies pressure against the bowel wall and can lead to autonomic dysreflexia and sympathetic discharge, especially in patients with a spinal cord injury.[4] Other potential complications include loss of anal sphincter tone, bowel perforation, and pressure necrosis of anorectal mucosa.[5] These are especially likely in mobile patients as movement can lead to alterations in pressure on the tubing and inhibit flow of fecal matter [6], further increasing bowel wall stress.
Conclusions: In our patient, her mobility and altered consciousness likely led to the self-removal of her rectal tube and ensuing complications. Although convenient, the risks and benefits of rectal tubes should be thoroughly evaluated on a daily basis to assess their continued need and to prevent complications that may increase morbidity.