Background: Patients who are frequently admitted to the hospital are a highly vulnerable population, facing discontinuity between hospital admissions and care settings. At the Hospital of the University of Pennsylvania, the multidisciplinary STEP program works intensively with patients with extreme hospital utilization on the inpatient general medicine service (minimum of 5 but often 10-30 admissions per year). Of enrollees in the first three years of the program, over half were 18-35 years old, and of these, over 80% were women. Our extended work with these patients led us to hypothesize that challenges faced at the time of transition from pediatric to adult care may have played significant roles in patients’ experiences and utilization over time.
Methods: In depth, semi-structured interviews were carried out with 11 women ages 18-35 who are currently or previously enrolled in the STEP program. 17 patients were identified as eligible for the study and 11 interviews were completed. Interviews were conducted by two medical students trained in qualitative interviewing. Most interviews took place in-person, during hospital admissions, with the remainder conducted over the phone. Questions were open-ended, designed to identify drivers of frequent hospitalizations, patients’ experiences with transition from pediatric to adult care, and patient perceptions of how their care could improve. Interviews were audio recorded, transcribed, coded, and thematically analyzed.
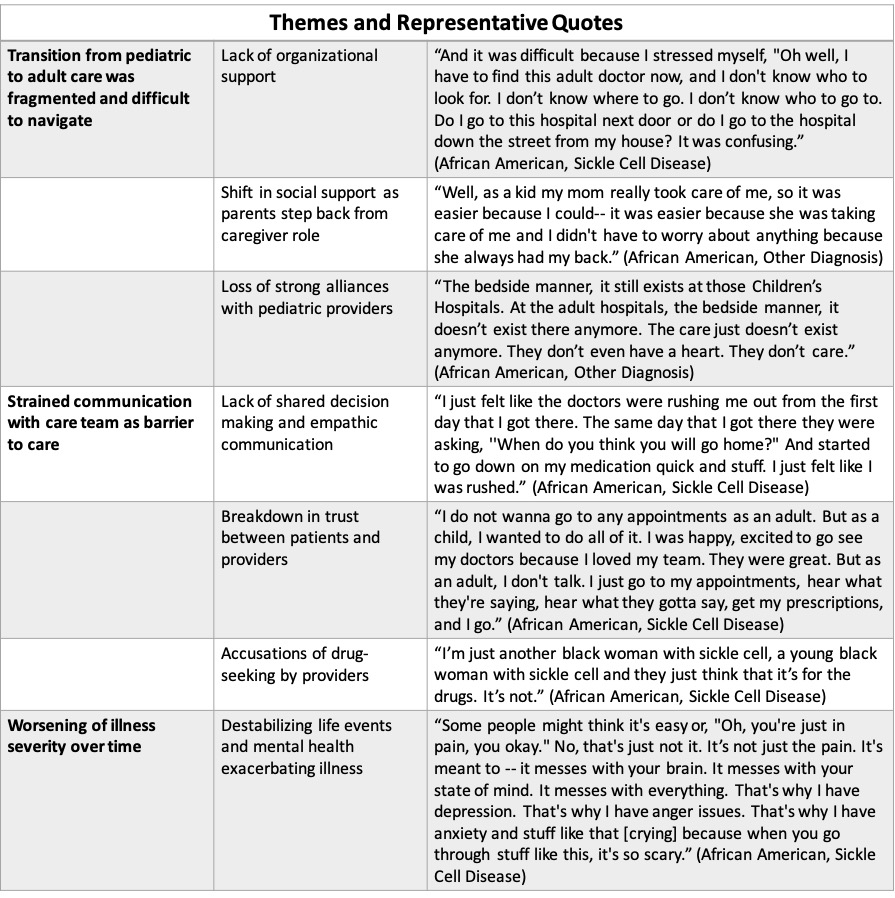
Results: Of patients interviewed, 64% have a primary diagnosis of sickle cell disease. Three primary themes emerged in interviews: lack of support in transition from pediatric to adult care with a decline in quality of care, strained communication with providers as a barrier to care, and decompensation in illness and worsening health as patients enter adulthood. All but one patient experienced difficulty transitioning from pediatric to adult care. Patients described strong alliances with pediatric providers, who they felt were more understanding of their needs. Study participants experienced fragmentation in care when transitioning to adult providers, facing delays and confusion when establishing a new outpatient team. Patients feel stigmatized by providers, particularly in regard to pain management. They feel their providers do not adequately involve them in clinical decision making and that they are discharged before their pain is adequately controlled. Over 70% of participants reported 2 or more Adverse Childhood Experiences (ACEs), with an average of 3.6 experiences.
Conclusions: The experiences and perceptions of participants in this study suggest multiple avenues for patient centered interventions that may improve care in this population, all based on improving communication and shared decision making between patients and providers. The experiences of these patients, and high utilizing populations in general, provide a window into the cracks in our systems of care; identifying these cracks can help us understand where the system can be improved not only for this specific population, but also globally to the benefit of all patients. One crucial area for improvement is the transition from pediatric to adult care. This transition represents a vulnerable time, during which many patients – and in particular those with history of ACEs – would likely benefit from additional structure and support to establish effective communication strategies and strong relationships with new adult care teams.