Background: Hospitalists rely on patients’ family members and caregivers to convey medical history, communicate on the patient’s behalf, assist with decision making, participate in care training, partake in discharge planning and provide support. With the rise of COVID-19 infection rates across the country, hospitals promptly enforced strict visitation protocols to prevent transmission, preserve PPE and maintain the health of staff members (1). Congruent with CDC Guidelines, our hospital implemented a visitation policy during the pandemic restricting visitors for hospitalized patients. Limited exceptions were granted for patients at end-of-life or with altered mental status. It is unknown how these policies impact experience. We conducted a survey of discharged patients to determine the impact of a restricted visitation policy on patient hospital experience.
Methods: A four-item questionnaire was administered by phone to randomly selected adult patients discharged between 3/15/2020 and 8/15/2020 from the Hospital Medicine service. Questions included: number of visitors allowed, communication about and awareness of the policy, and impact of the visitation policy on hospital-stay. Demographic information, including COVID-19 status, was obtained through review of electronic health record. Descriptive statistics and 2-sided χ2 analyses were performed. The study was IRB approved.
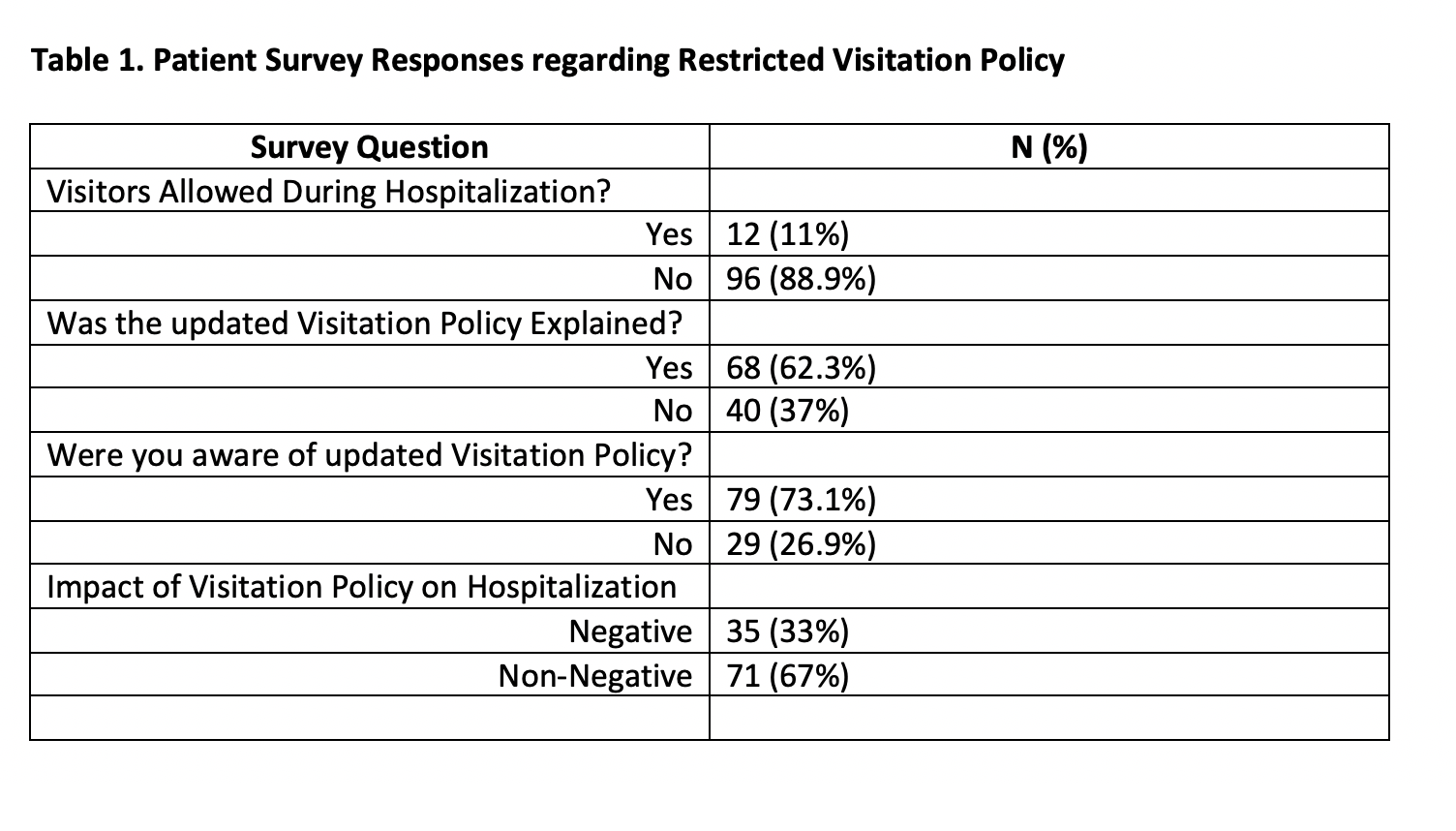
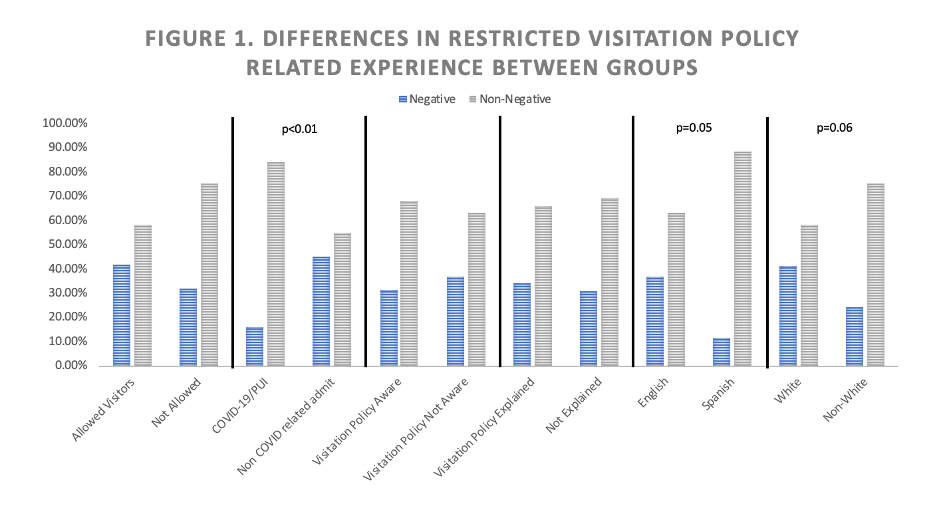
Results: 108 patients completed the survey. 31.4% identified as Hispanic and 14% were Spanish speaking only. 38.8% of respondents were COVID-19/PUI (person under investigation). The majority of patients (88.9%) were not allowed visitors. 73.1% reported being aware of the updated visitation policy. 33% reported a negative impact of the visitation policy on hospitalization. There was no difference between patients who were allowed a visitor compared to those who were not. A significant difference was found between patients admitted as COVID-19/PUI compared to those who were not, with only 16% of COVID-19/PUI reporting a negative impact compared to 45.2% of non-COVID admits (p<0.01). A significant difference was found between English and Spanish speakers (37% vs. 11.8% reporting negative impact respectively (p=0.05)). A trend towards significance was found between White and non-White, with non-White reporting less impact (p=0.06). There was no significant difference for awareness of the policy or recall of having it explained.
Conclusions: Our study found that almost one third of patients experienced a negative impact of strict visitation policies on hospitalization. This impact was not affected by awareness of or explanation of the policy. COVID-19/PUI were less likely to report a negative impact from limited visitation policies compared to other diagnoses, perhaps related to substantial transmission risk and fear of infecting loved ones related to their diagnosis. Results also demonstrated that Spanish speaking and non-White patients were less likely to report negative impact. Studies suggest that flexible visitation decreases patient delirium and anxiety and improves family member satisfaction (2). With no end to the pandemic in sight, restrictive visitation policies will continue to affect hospitalists and their patients. Hospitalists will need to develop new workflows and standard practices to bridge the gap left from visitation restrictions. Attempts to mitigate this impact may include standing phone calls or video visits with family members and daily consideration if patient meets exception criteria.