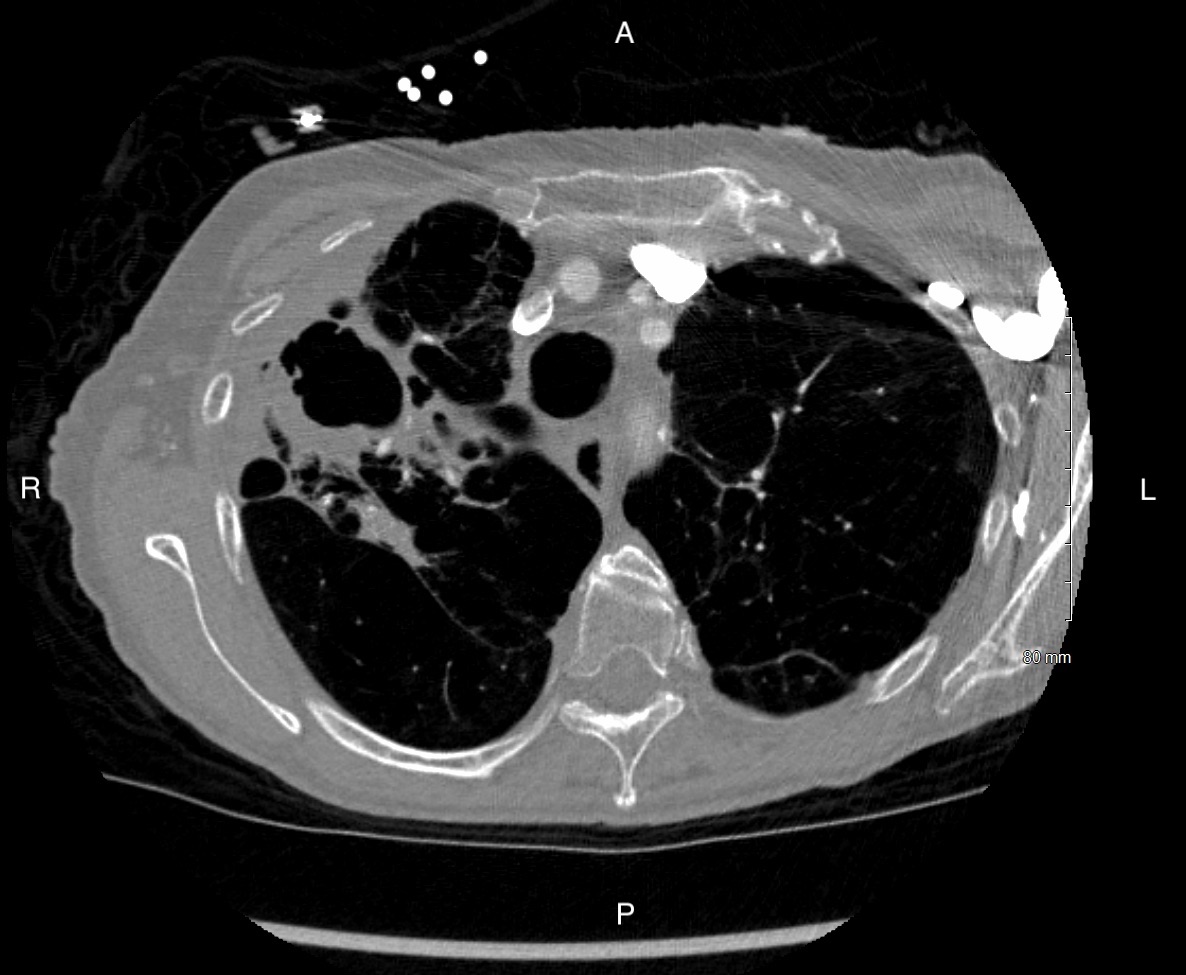
Case Presentation: Pulmonary hypertension (PH) affects 1% of the global population, including 10% of people over 65 and ~50% of people with Congestive Heart Failure (CHF). Pulmonary hypertension (PH) is classified into 5 clinical subgroups: pulmonary arterial hypertension (PAH), PH due to left-sided heart disease, PH due to chronic lung disease, PH due to chronic thromboembolic disease (CTEPH), and PH with idiopathic or multifactorial etiology. A 75 Y female with a PMH including severe COPD on 6-7L home O2 and MAC infection, presented with 5 days worsening exertional dyspnea, increased O2 requirement, and chest “tightness” with exertion. She was afebrile, HR 87, RR 36, BP 153/103, SaO2 98% on 5L NC. Physical exam was significant for respiratory distress with mild accessory muscle use, without wheezing or crackles, and 1+ peripheral edema to just above the ankles. Labs included a troponin of 43 and BNP of 11,319 (increased from 3,344 one month prior). Initial diagnosis was new onset CHF exacerbation, and the patient was treated with IV furosemide. A CT PE scan showed centrilobular emphysema and non-TB MAC that progressed from nodules to thick-walled cavitary lesions. The CT scan was negative for VTE, significant pulmonary congestion or acute PE, though V/Q scan is gold standard for CTEPH. After 2L of diuresis, an echocardiogram showed an elevated PA pressure of 82 mmHg. Mean PA systolic pressure increased from 30 to 38 mmHg from the patient’s most recent RHC (10/2019). The PVR also increased from 5 to 11 Woods units.
Discussion: Though the patient has severe COPD, her PH was most likely due to group 1 rather than group 3 PH, as the PA pressure increased beyond what would be expected in one year solely from COPD. The patient was started on a vasodilator used in group 1 PAH.
Conclusions: This case highlights the difficulties of diagnosing pulmonary hypertension. PH is often initially mistaken for a CHF exacerbation. In addition, the etiology of PH can be difficult to diagnose. However, accurate diagnosis and classification is essential for effective therapy, as treatment can be targeted to the specific type of PH. Reclassifying this patient as group 1 PAH opened medication options that are efficacious in group 1, but not group 3 PH.