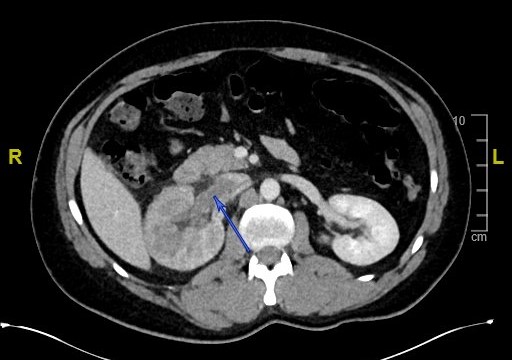
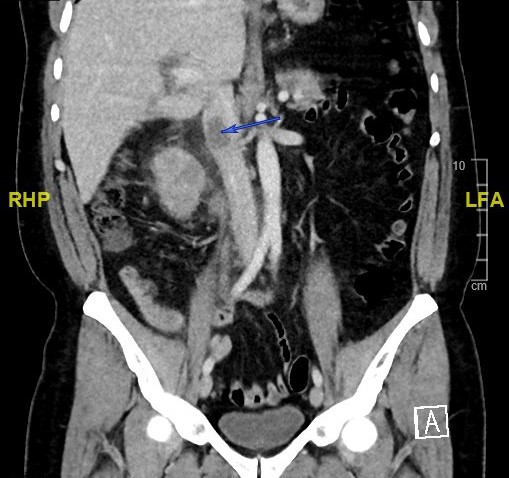
Case Presentation: A 45-year-old male with no significant past medical history and on no medications presented to the Emergency Department with two-day history of an acute onset of intermittent non-radiating diffuse abdominal pain and hematuria. Two weeks prior, he tested positive for SARS-CoV-2 and was on self-quarantine at home. He had been feeling better until two days prior to admission. He denied fever, chest pain, dysuria, vomiting or diarrhea. He had no family history of malignancy and denied use of alcohol, tobacco or illicit drugs. The patient had normal vital signs and his physical examination was unremarkable with no abdominal or costovertebral angle tenderness. His coagulation panel was normal. He had mild leukocytosis of 12k/uL, serum creatinine of 1.3mg/dl (normal 0.5-1.3)) and mild transaminitis. CT angiogram of his abdomen and pelvis demonstrated decreased enhancement of the right renal vein (Images 1 and 2). A follow-up doppler ultrasound of the renal vein suggested a right Renal Vein Thrombosis (RVT). Urinalysis revealed numerous red blood cells with mild bacteriuria, 30mg/dl protein and pyuria. A hypercoagulability workup was negative for prothrombin gene, factor V Leiden mutation and anti-cardiolipin IgM was low positive at 60.5MPL (<12.5). The cause of his abdominal pain and hematuria was secondary to RVT possibly due to hypercoagulability from his COVID-19 infection. He was treated with intravenous heparin; his hematuria resolved and was discharged to home on direct acting oral anticoagulant. Patient was advised further work up of additional hypercoagulability and repeating anti-cardiolipin antibodies in twelve weeks as an outpatient.
Discussion: Acute RVT is often due to trauma, severe dehydration, hypercoagulability or nephrotic syndrome. Patients with SARS-CoV-2 infection are at significant risk of developing arterial and deep venous thrombosis which can develop in almost any location. Literature search has shown that coagulopathy in these patients is due to the inflammatory response to SARS-CoV-2. It might infect endothelial cells causing diffuse endothelial inflammation and microvascular damage resulting in widespread thrombosis [1]. Antiphospholipid (aPL) antibodies were detected in 52% of patients with COVID-19 and are potentially pathogenic [2]. Acute RVT presents as abdominal pain with hematuria. Diagnosis is by CT angiography or MR venography. Treatment of acute RVT without Acute Kidney Injury (AKI) is therapeutic anticoagulation unless contraindicated and those with AKI should undergo thrombolysis with or without thrombectomy [3]. Duration of anticoagulation is usually six to twelve months.
Conclusions: This case reflects a rare presentation of an acute RVT in SARS-CoV-2 infection and a high degree of suspicion should be maintained to rule out RVT in these patients who develop abdominal pain and urinary symptoms. A close follow up is needed to see if aPL antibodies are transient or persistent in patients who recover from COVID-19 and their future risk of thromboembolism.