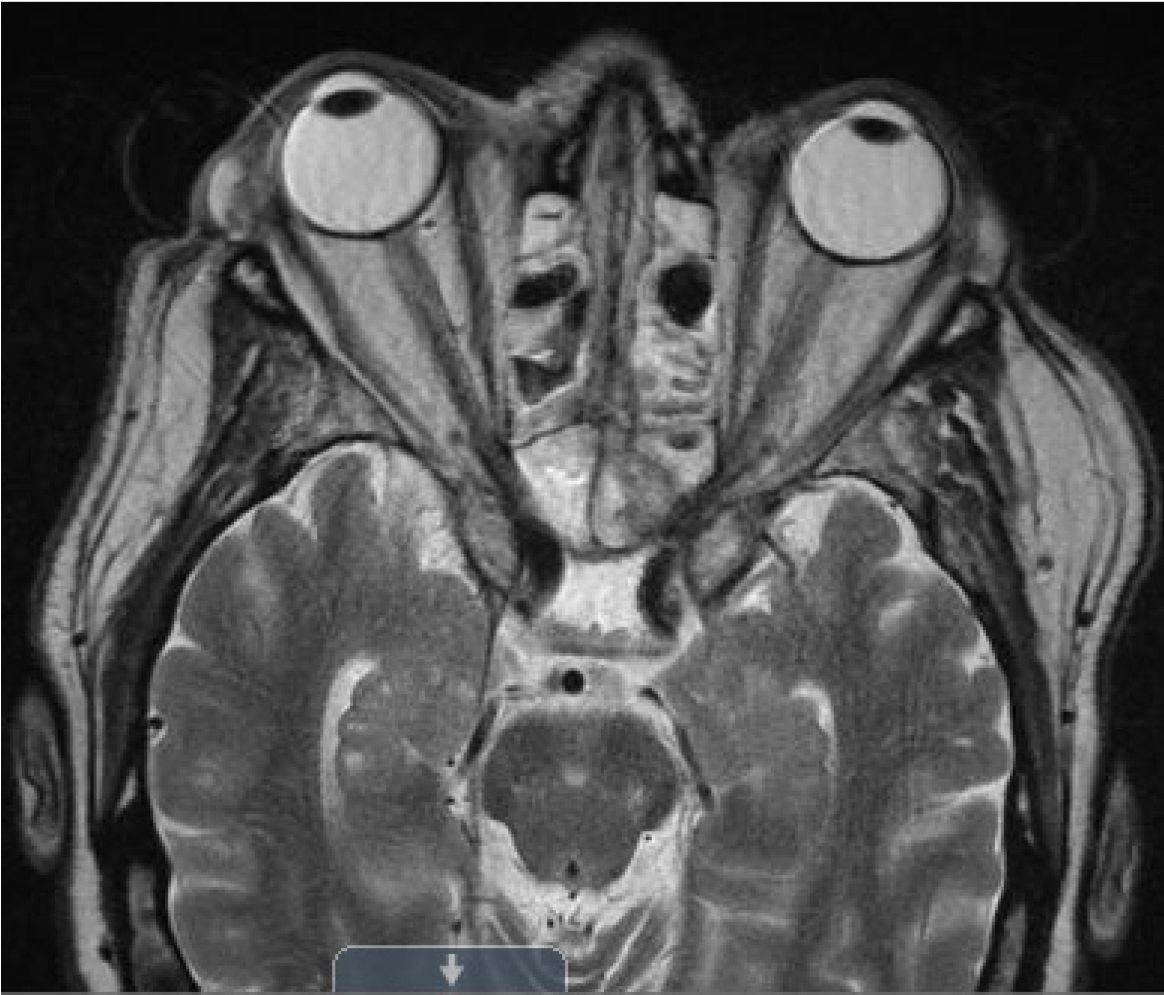
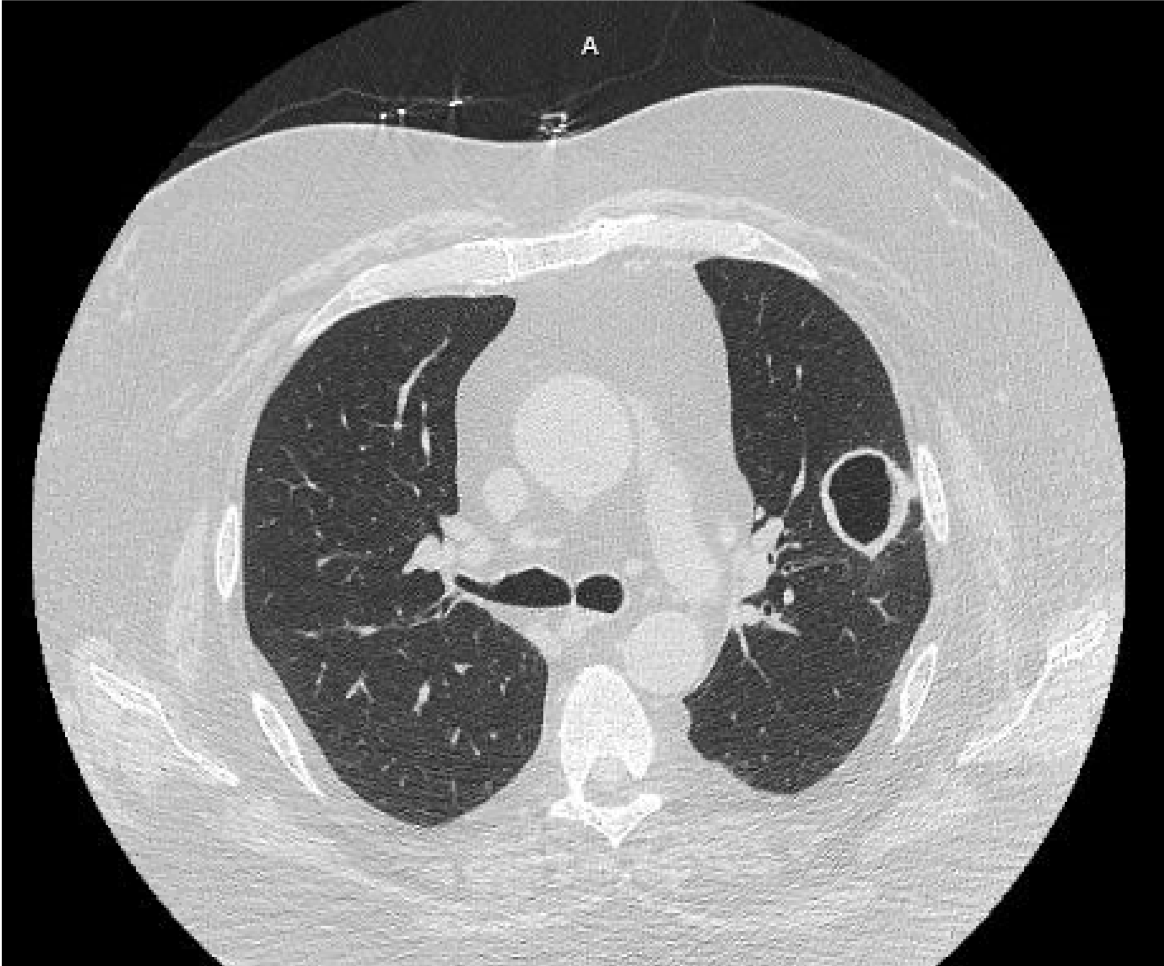
Case Presentation: A 60-year-old man with no history of diabetes presented with right sided facial swelling and was found to have HbA1c of 14%. He was treated for sinusitis with augmentin and discharged with close follow-up for new-onset diabetes mellitus type 2. A few days later, he developed new left eye blindness necessitating readmission. On readmission, vitals were notable for atrial fibrillation with heart rate 96 beats/min. On exam, he had right sided peri-orbital edema, tenderness over right maxillary sinus, complete loss of vision in the left eye with no pupillary reaction, and large black eschar over the hard palate. Initial labs were remarkable for HbA1c of 18.9%, WBC 6.9K, glucose 103, and chest x-ray with a cavitary lesion in the left upper lobe. Palatal fungal cultures grew Rhizopus, Candida glabrata, and Candida intermedia. Blood cultures were negative with absence of vegetations on transthoracic echocardiogram. Patient was started on vancomycin, cefepime, clindamycin, amphotericin B, and micafungin. He underwent emergent sinusectomy, septectomy, ethmoidectomy, sphenoidectomy, and turbinectomy with serial aggressive debridement. Intraoperative specimen showed 90-degree branching invasive fungi consistent with mucormycosis. A left upper lobectomy demonstrated extensive necrosis and angioinvasive fungal organisms, confirming pulmonary involvement. Despite these interventions, patient developed internal carotid artery thrombosis complicated by mycotic emboli resulting in subacute infarcts of the left frontal, parietal, and occipital lobes. He was ultimately transitioned to comfort care and expired in the hospital.
Discussion: Mucormycosis, commonly caused by Rhizopus oryzae, is a life-threatening fungal infection affecting immunocompromised patients. Despite aggressive surgical debridement and antifungals, it has over 50% mortality rate. Mucormycosis originates from paranasal sinuses, invades the blood vessels, and disseminates to other organs including the lungs. The hyphae form thrombi, which can lead to tissue necrosis. Rhizopus is the predominant pathogen, most commonly affecting the rhinocerebral region. However, it can affect many organ systems, including the lungs which is associated with a 75% mortality rate. The most important risk factors for mucormycosis are uncontrolled diabetes, malignant hematological disease, long-term corticosteroid therapy, organ transplant, and severe neutropenia. As in our patient, initial presentation can be nonspecific with headaches, facial cellulitis, nasal discharge. Definitive diagnosis is made with tissue biopsy showing nonseptae hyphae with 90-degree angle branching. Emergent surgical intervention with adjunctive antifungals is imperative as this disease carries a mortality rate of greater than 50 percent despite appropriate therapies.
Conclusions: 1. Consider invasive mucormycosis in a patient with new onset or poorly-controlled diabetes, facial swelling, and headache. 2. Recognize the need to initiate urgent surgical debridement and amphotericin B in suspected rhinocerebral and pulmonary mucormycosis.