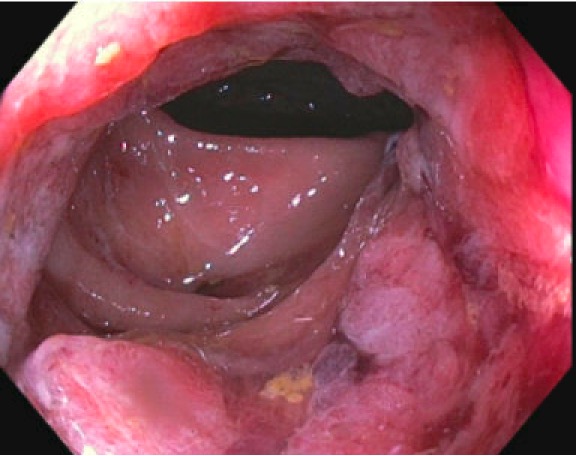
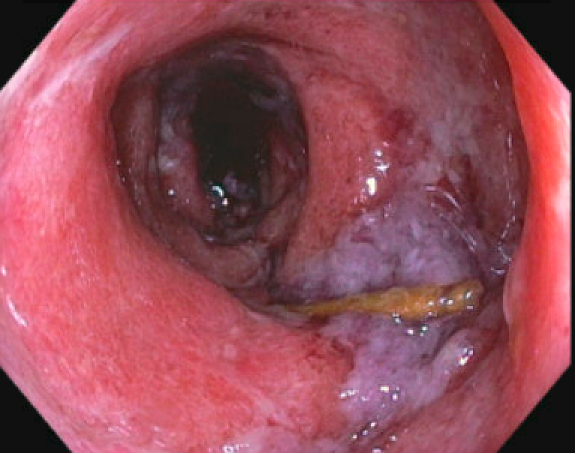
Case Presentation: A 76-year-old female with a history of an incarcerated hernia, Clostridium difficile colitis, hypertension, and dyslipidemia presented to the emergency department (ED) with bloody diarrhea and weakness. On admission, the patient denied fevers, chills, or cough. Additional symptoms included self-limited hyponatremia (133 mmol/L), likely due to excessive diarrhea, bleeding internal hemorrhoids with discomfort, and worsening postprandial abdominal pain. A colonoscopy revealed severe Cytomegalovirus (CMV) colitis in the rectum. Immunology work up confirmed a positive CMV IgG, along with a negative HIV screen and CD4 count (885 cell/mm3), IgA, IgM, and IgG within normal limits. Patient improved with treatment and was discharged to complete a six-week course of Valganciclovir. Two weeks later, patient presented to the ED for abdominal pain and shortness of breath. She reported new-onset lower quadrant cramping pain and watery stools. Labs were significant for an elevated BNP (2000 pg/mL). TTE revealed a newly reduced EF of 33%, which along with wall motion abnormalities were suggestive of stress cardiomyopathy. Her overall condition during this hospitalization quickly worsened. Although she was offered intubation and ICU care, given the generally reversible nature of stress cardiomyopathy, the family elected for inpatient hospice and comfort care in accordance with her wishes. Patient died a few days later.
Discussion: Cytomegalovirus is a DNA virus prevalent in much of the population but remains asymptomatic in the immunocompetent population. It can present as colitis amongst other clinical manifestations in immunosuppressed patients. Clinical manifestations of CMV can largely vary, as healthy individuals are typically asymptomatic or present with mononucleosis. Conversely, CMV takes a more aggressive approach in immunocompromised individuals by causing hepatitis, retinitis, esophagitis, and colitis [1]. 40-100% of the world’s population is estimated to be seropositive for CMV [2]. In patients with severe colitis, CMV reactivation appears to be the etiology in 4.5 -16% [3]. The prevalence of CMV colitis in immunocompetent people is unknown as there are only a few anecdotal reports [4]. Symptoms usually include diarrhea, hematochezia, abdominal pain, fevers, weight loss, and malaise [5]. A recent meta-analysis on CMV colitis in the immunocompetent highlighted important risk factors that affect morbidity rates.5 Male gender, advanced age, and comorbidities are imperative in determining prognosis and overall outcomes [4]. Of the 32% of people who died, 100% were older than the age of 55 [5]. Treatment of CMV colitis is often forgone in patients with intact immune systems due to the myriad of side effects caused by antiviral agents. There is insufficient research regarding the effectiveness of antiviral agents in treating CMV colitis. The drug of choice remains oral or IV ganciclovir [6]. Further research is warranted to define subgroups that would benefit from therapy.
Conclusions: The aim of this report is to draw attention to the rare presentation of colitis in an immunocompetent patient and encourage clinicians to recognize important risk factors. It is crucial to do a thorough workup to identify immunosuppression, as well as underlying etiologies that could likely explain the demise of this patient months later.